Spinal care following surgery
This brochure is relevant for all persons undergoing spinal surgery of any type. Although there is much reference to the lower back, maintaining these principals will also protect the upper back and neck. It may also be appropriate for non surgical back conditions.
Spinal Anatomy
The spine is a complex structure consisting of bones (vertebrae), intervertebral discs, ligaments, nerves and muscles, which allow for both mobility (movement) and stability (protection).
The spinal column is made up of 33 individual vertebrae, which are divided into five areas: cervical (neck), thoracic (upper back), lumbar (lower back), sacral, and coccyx (tailbone). The spine does not run straight up and down, but has three natural curves to help spread the load.
Between each vertebra is a disc. The discs allow movement between the vertebrae, but also help to absorb load from activities such as bending and lifting. Each disc has a soft centre (nucleus) surrounded by tough fibrous outer rings (annulus). Healthy discs are elastic and springy.
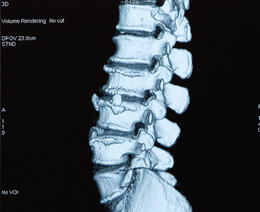
Excessive or abnormal loading of the spine can cause degeneration (wear and tear) or injury (e.g. bulge or prolapse) of the disc. There are numerous ligaments running between the vertebrae along the length of the spinal column. They resist excessive movement, and therefore help to provide stability to the spinal column.
The muscles of the spinal column have two main functions. The superficial muscles allow and perform movement of the spine. Your deep core stability muscles provide protection and stability for the spine. These muscles include your transversus abdominus (deep tummy muscle), diaphragm, pelvic floor and multifidus (deep back muscle). Research has shown that following an episode of lower back pain these muscles lose their efficiency at stabilising the back and pelvis.
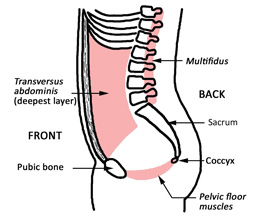
Image: Core Stability Muscles. Pelvic Floor Recovery. © Sue Croft Physiotherapy.
They do not automatically regain their strength when the pain goes away. This makes your spine vulnerable to future episodes of back pain. Specific deep stability exercises will help to reduce your pain, increase your function, and help prevent further injury. General exercise such as walking or swimming will not specifically strengthen your stability muscles, although down the track general exercise and strength will be important. These specific stability exercises will commence in hospital. Your physiotherapist can assess the function of your stability muscles with the use of ultrasound imaging and show you more challenging exercises as your contraction improves. This is done at the physiotherapists' rooms usually two to three weeks after surgery.
The spinal cord runs down the spinal column through the spinal canal, which is formed by the vertebral arch (lamina). The spinal nerves exit the spinal column through side openings (foramen) formed by adjacent vertebrae. The nerves carry information between the brain and the rest of the body. This information includes outgoing movement commands to muscles and incoming sensory information from skin, muscles and joints.
The nerves can become irritated or compressed when there is insufficient space for the nerve to exit the spinal column (stenosis). This may be due to a disc injury, bony changes, or the presence of inflammation. This can cause symptoms such as pins and needles, numbness, or pain in the legs. The degree that these symptoms will ease after back surgery depends on the individual, the extent of the compression, and the length of time the symptoms have been present. Nerve pain can resolve quite quickly after surgery but can take a bit longer if the damage was more severe.
How long will it take to fully recover from surgery?
Everybody recovers from surgery at a different rate. Recovery will depend on:
- the type of surgery you have undergone
- your general health status, i.e. other medical problems
- your general musculoskeletal status, i.e. general muscle control and strength fitness level
- the degree of symptoms at the time of surgery.
General soft tissue healing rates
The human body heals with the laying down of connective tissue, often called scar tissue. Healing rates vary between individuals but generally at four weeks connective tissue has reached 60 per cent strength, at six weeks it is at 80 per cent and by 12 weeks, it will have regained 100 per cent strength.
However, the control, strength and endurance of the supporting muscles of the spine, shoulder and pelvis can take longer.
Surgery types
Discectomy/laminectomy—if you have had a discectomy the recovery rate is between three and six months. Soft tissue such as muscle, ligament and disc takes 12 weeks for full healing to take place. You should not be doing any heavy lifting before this time.
Fusion/disc replacement—if you have had a fusion or replacement, recovery rates are between six and 12 months, as full bone healing can take 12 months. Neck surgery commonly involves a fusion. If you are not sure what has been performed, please speak to your doctor. These are estimates only. Your recovery may be faster, or take longer. Do not be alarmed if you are slow to heal, as everybody is different.
Minimally Invasive Surgeries may have reduced pain levels associated with surgery, allow more comfortable movement and an earlier return to function in some cases. The wound is much smaller and the spinal biomechanics maybe disrupted less. However, connective tissue healing rates are the same. Some of the timeframes for return to activity that follow, may be reduced as your pain allows.
General health
Age—unfortunately it is true the older you are the longer you will take to recover.
Fitness—the higher your general fitness levels before your surgery, the faster you will recover. It is never too late to start to improve your fitness. Even a small improvement will enhance your recovery.
Muscle control—the better your muscle control, strength and endurance, the better your recovery. Your physiotherapist may be able to advise you how to achieve this. It is never too late to start to improve your muscle control, although pain may inhibit you from performing some exercises. Even a small improvement in available muscles will enhance your recovery.
Breathing control—correct breathing patterns have a direct impact on spinal muscle control. Breathing should be relaxed with air drawn into the bases of the lungs with long slow breaths out. Relax the neck muscles.
Symptoms pre-op—severe leg symptoms causing weakness or numbness may result in a longer recovery. Severe back pain before your surgery may also take longer to resolve.
Smoking—numerous studies have consistently shown that smoking is associated with slower healing rates and poorer prognosis after surgery. If you cannot quit smoking, cutting back would assist your recovery from surgery. Visit the Quit Campaign website (http://www.qld.gov.au/health/staying-healthy/atods/smoking/) for further information.
Medical health—other existing medical conditions such as diabetes will also slow your healing rate. In order to maximise your recovery and assist in preventing future complications, these healing times should be kept in mind when increasing physical activity. Do not be tempted to overdo it just because you are not experiencing pain. If your leg or back symptoms recur, reflect on what activities you have been doing over the preceding days. Reducing activity in the early stages usually allows symptoms to settle. If they persist even after rest, please speak to your doctor or physiotherapist.
Positioning
These tips will help to reduce pressure on your spine pre and post operatively.
They should become long-term strategies.
Lying
- Ensure that your mattress has sufficient support (medium firmness) and your pillow is not too thick or too flat (your neck should be in the midline position).
- Try to keep your spine as straight as possible (i.e. not twisted or side bent), although your legs and hips may be bent.
- Never lie with your head and upper trunk elevated with the legs out straight. This will increase the stretch on the neural structures, which may increase pain in the spine and/or limbs.
- You may lie on your back or on your side, but not on your stomach.
- You may be more comfortable placing a pillow between your knees if lying on your side, or under the knees if lying on your back.
- Wearing satin pyjamas/underwear/boxer shorts can make it easier to change position in bed.
- Neck/upper back surgery—the bed head is elevated 20 to 30 degrees for 24 to 48 hours for swelling. Keep the knees bent to reduce strain on the spinal cord. Use a pillow under knees. Resume normal flat bed position ASAP or very slight elevation only.
Lower back surgery—keep the electronic bed head down. Flat is best and keeps the back straight. Lifting the bed head is equivalent to bending forward at the waist and can bring on leg pain. Hospital staff can tilt the entire bed if required.
- If you have your own posture pillow or favourite pillow from home we recommend you bring it with you for comfort.
Getting out of bed
- Bend your hips and knees and roll onto one side keeping your spine straight and your knees together.
- With the knees bent bring your feet to the edge of the bed.
- Push yourself up sideways and drop your feet over the edge.
- Take a few breaths on the edge of the bed and move your feet before standing up. Do not stand up if you feel light-headed or nauseous. If the symptoms do not settle, lie back down on your side again.
Sitting
Sitting is limited to 20 minutes at a time for the first two weeks after surgery. This is increased to 40 minutes by four weeks. You should return to bed or go for a short walk if you start to feel uncomfortable. Periods of sitting can be repeated many times a day with a rest lying down in between for 30 to 60 minutes.
For good sitting posture:
- Ensure feet are on the ground. Legs must not be elevated in an extended (straight) position on a stool, as this increases the stretch on the neural structures. Do not cross your legs (see computer tips).
- Your knees should be just below the height of the hips
- Ensure you are centred in the chair, and not leaning to one side.
- Gently tilt your pelvis forward so that you are not slouching back onto your tailbone. A pillow can be placed behind the back for comfort and to keep the spine straight.
- Gently draw your shoulder blades back, opening out the front of the chest.
- Gently lift the back of your skull off the top of your spinal column (think tall). Ensure your chin is not poking out.
- Avoid the use of recliner chairs—they offer no spinal support, and have negative effects on muscle strength and balance if used in the long term.
After four weeks, sitting tolerances will increase to an hour or more. However studies show that breaking up your sitting time (by standing up every 30 minutes or so) can reduce risk factors for developing heart disease and diabetes, in addition to the positive impact changing positiotn has on your muscles and spine. Keep moving.
Alternating positions
Alternate tasks and change positions to reduce fatigue and tension. Remember to take frequent breaks if you are doing a single task for a prolonged period (e.g. every 10 to 15 minutes).
Standing
Good posture is essential following back surgery—it places less load on the spinal joints and nerves, and helps to recruit your stability muscles.
For good standing posture:
- stand with your feet hip width apart
- ensure there is weight going through both heels (do not stand with your weight all on one leg, or with weight through the balls of your feet)
- relax your knees
- gently draw in your lower tummy (transversus abdominus) and pull up your pelvic floor
- gently draw your shoulder blades back
- gently lift the back of your skull off the top of your spinal column (think tall)
Wearing high heels should be avoided. High heels place more load on the legs and spine, and can cause tightening of the calves and hamstrings, and weakening of the spinal muscles.
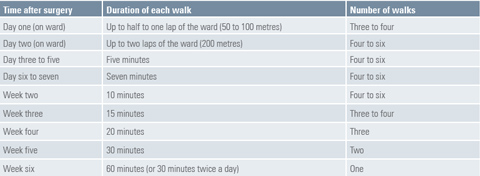
Walking programs
Being active is the key to optimal recovery. Physical fitness and conditioning have a significant impact on preventing and reducing the effects of back injury. A graduated walking program begins immediately after your back surgery.
There are many benefits to walking including:
- improved mood and stress relief (exercise stimulates the release of the body's endorphins). As a result, you should feel better during the day, and sleep better at night
- improved heart and lung function, and improved circulation
- improved general muscle activity and spinal mobility
- improved bladder and bowel function
- facilitation of weight loss in conjunction with a healthy diet. Reducing weight, particularly around the abdomen and pelvis will assist in reducing the stress on your spine.
- improved balance and posture.
Walking is a low load activity that should be suitable for most people. Ensure that you wear good supportive shoes (e.g. running shoes that are not worn out). You may need assistance to put on your shoes for the first two weeks after surgery. Start with a comfortable pace and gradually increase speed. Avoid hills initially if possible. The table below is a general guideline for a walking program, but it will vary between individuals. If you have any concerns with the program, discuss these with your physiotherapist.
Getting home from hospital
If you live within 100 to 200 kilometres of Mater Private Hospital Brisbane, you may be driven home. Otherwise, flying is recommended (unless the trip can be broken into stages).
By car:
- Break the trip every 30 to 45 minutes.
- Stretch your legs and walk intermittently, or lie down.
- Use extra flat pillows for extra support.
- You can recline your seat back a little but your seat belt must still be effective.
- Stay hydrated, eat fibrous foods and other strategies to avoid constipation.
By air:
- Prearrange assistance with baggage.
- Alert airline staff so you can get onto the aircraft last and get off first.
- If sitting is uncomfortable, organise an aisle seat and stand up during flight if it is safe to do so.
Getting into the pool
It is recommended that you start exercising in the pool from 10 to 14 days after your operation (when the wound looks healed). Exercising in the pool has the benefits of reducing the load on your joints (due to the effect of buoyancy), relaxation of muscle tension, improving cardiovascular fitness, spinal mobility and muscle strengthening. Start with gentle walking in the water. This can be progressed to walking sideways and backwards, gentle squats, sitting on the step and cycling legs etc. Just standing in the water propelling your arms in all directions whilst keeping your body still is another option you can try. You can start 10 freestyle and backstroke laps from three to four weeks after your surgery. Breast-stroke should be avoided for the first three months.
Bladder and bowel care
Good bladder and bowel habits are essential following spinal surgery.
Ensure that you:
- avoid "just in case" visits to the toilet
- limit caffeine and alcohol intake
- avoid constipation or straining (bearing down). Consuming pear or prune juice may assist with easing constipation
- be a non-smoker
- exercise regularly (e.g. walking)
- ensure you are at a healthy bodyweight. An increase in weight places extra pressure on your pelvic floor
- ensure good consistency of stool (soft and easy to pass) by adequate fluid intake (drink six to eight glasses a day) and eating high fibre foods (e.g. fruits, vegetables, wholegrain breads and cereals, sprinkling psyllium husk on your cereal)
- be committed to doing your pelvic floor exercises (see below).

Correct toilet positioning
This is necessarily different to other seating positions described earlier.
Ensure you sit properly on the toilet—do not hover. The ideal position for emptying your bladder and bowels is as follows:
- have your knees higher than hips
- have your feet apart on the ground or a small stool
- keep your back straight by maintaining the normal inward lumbar curve. Flattening the back, i.e. tilting it backwards will reduce the openings for the bladder and bowel.
- tilt your trunk forward at your hips
- lean your hands on knees
- allow your abdomen to relax forward
- do not hold your breath or bear down
- gently increase pressure within the abdomen and sustain the pressure whilst breathing.
Continue using this position as a lifelong habit.
The pelvic floor is an important component of bladder and bowel management for both men and women. The pelvic floor is a muscular sling across the base of the pelvis. It supports the bladder, bowel and reproductive organs. Signs of a weak pelvic floor include:
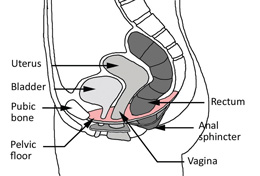
- any leakage of urine with extra pressure (e.g. coughing, sneezing, jumping)
- increased frequency—passing urine more than six to eight times a day and more than once at night
- an urgent need to pass urine
- problems controlling bowel contents, chronic constipation, or difficulty opening bowels
Pelvic floor exercises can be very effective in improving bladder and bowel function. Try this exercise to start strengthening your pelvic floor:
- lie on your back with knees bent and feet on the bed/floor. Keep your spine straight. Slowly draw up your pelvic floor around your urethra (as if you are stopping the flow of urine) and back passage
- keep breathing as you hold
- start with a five second contraction and gradually build up your holding time
- aim to do the exercises frequently (e.g. four to six times a day).
- try the exercise in various positions once you can master a pelvic floor contraction lying down (e.g. standing in line at the supermarket, sitting in the car at traffic lights etc.)
Remember, good posture will help to recruit your pelvic floor muscles.
Tips for correct lifting
You should not be lifting anything heavier than a couple of kilograms for the first four weeks or heavier than 10 kilograms for the first three months following surgery. Some simple guidelines should be followed:
- Never lift a weight you do not feel comfortable lifting.
- Check the environment for obstacles first (de-clutter).
- Draw in your transversus abdominus (lower tummy muscle) before and during a lifting manoeuvre.
- Never bend at the waist. Stand close to the object with the feet apart and bend at the knees. Secure your grip, then push up with your legs while keeping your back straight.
- Carry objects as close to your body as possible to minimise stress on the spine. If the object is very large, ask someone else to help you.
- Avoid repetitive lifting (even of light weights)—break your task up into short periods. After back surgery you will fatigue very quickly, which increases your likelihood of injury.
- Never twist while lifting or carrying.
- Place buckets, clothes baskets etc. on a stool or bench to fill. This will avoid the need to lift heavy objects off the ground.
- Never lift heavy or large furniture.
- Balance any loads you carry, eg. a shopping bag in each hand.
- Remember that pushing places less strain on your back than pulling.
- Overhead or any lifting above shoulder height should be restricted, especially if you have had neck or upper back surgery. Over head lifting increases the pressure through the discs in the neck and a number of shoulder muscles attach to the neck itself which is trying to heal. You should avoid hanging out awkward or heavy items on the clothes line for the first six weeks. Lifting pots and pans into overhead cupboards should also be avoided during this time.
At 12 weeks you can perform these tasks, including light resistive work. However heavy lifting (more than 20 kilograms for men and more than 10 kilograms for women) and any repetitive lifting (more than 10 kilograms for men and more than five kilograms for women) should be permanently avoided to reduce the risk of damage to the discs above and below the surgery site.These approximate limits will be dependant on your age and physical capacity.
If returning to weights at the gym shoulder press and lat pull down should be performed with light weights and good alignment. If you have had upper spinal surgery, lat pull down needs to be to the chest not behind the head.
Tips for gardening
Although gardening is a popular hobby, people with a history of back problems need to take extra care. Bear in mind the healing times after surgery. You should not garden the first two months, and then only gradually begin gardening activities. The following advice should be used as a guideline:
- Do your spinal mobility exercises before starting your gardening to "warm up" your muscles and joints
- Break your time in the yard up into shorter periods (e.g. 15 minutes at a time)
- Vary your activities so that you are not in the same position or doing the same movement for a long period
- When doing tasks at ground level, kneel or use a low stool, rather than bending at the waist
- When lifting buckets/pots etc., bend your knees rather than your back—Do not fill the buckets to the top
- If the garden beds are wide, step into the garden bed rather than leaning into it from the edge
- Avoid repetitive twisting motions such as raking and shovelling for three months. After this time, move your feet to change direction rather than twisting through your trunk. If you feel you have not strengthened your spine sufficiently or have chronic back problems, do not attempt heavy work, such as digging or shovelling
- Use a wheelbarrow to transport heavy items rather than carrying them
- Use light-weight, well-designed tools
- Do not undertaken any lawn mowing for the first three months following surgery
- With neck surgery, avoid overhead pruning and chopping or sawing branches for 12 weeks. After this time, take frequent breaks when performing these tasks. In the early stages after surgery, listen to your body—if it hurts, do not do it (this may not necessarily be the case a few months after surgery. You should discuss this with your physiotherapist).
Tips for working at a computer

Remember that your 20 minute sitting limit applies when you return home. Working at a computer should be broken up into short periods—you may need to set an alarm to remind you to stand up. It is easy to get absorbed in your task and lose track of the time. Set up your workplace to minimise the stress on your back. This is a habit that should be sustained long after recovery from surgery.
- Sit with both feet flat on the ground (you may need to use a low stool). Your hips should be just higher than your knees, and you should have equal weight through both hips. With your hips at the back of the chair, the front of the seat should not place pressure on the backs of your knees or calves.
- Never cross your legs.
- Adjust the backrest to support your lumbar spine (at waist level). If your seat is not adjustable, use a folded/rolled towel or pillow for support in the small of your back.
- Your desk height should be just lower than your elbows (you may need to raise the seat height and place a stool under your feet).
- Wrists and hands should be in a relaxed position on your keyboard. The keyboard should be close to the edge of the desk so that your elbows hang vertically. Ensure your shoulders are relaxed.
- Your computer screen should be at eye level. If it is too low, your neck and back will be flexed, increasing strain on the spine. You may need to prop your screen up on a phone book. If you use a laptop, prop it up to the normal height of a computer and use a second, detached keyboard.
- Avoid sitting with the trunk and neck rotated to view your documents—work directly facing the computer. Use a document holder to elevate your files and place it as close to the screen as possible. If you are repetitively looking to one side, you should alternate the side at which your document folder sits. For documents that need to be written on, slightly raise the top end to create an upward slant.
- Be aware of neck position if bifocals are used. Task specific reading glasses may be necessary.
- After back surgery, do not sit on a theraball (exercise ball) at your computer. You will not have sufficient muscular endurance to maintain a good spinal position for an extended period while working initially.
- If you spend a lot of time on the phone, use a hands-free headset.
Tips for driving
Driving is not permitted after back surgery for the first three to four weeks. This is due to the lack of spinal control while sitting. Your insurance company may not cover you for driving less than four weeks after surgery.
When you start driving again:
- limit driving to short periods (no more than 20 minutes at a time)
- use a lumbar support in the small of your back ensure your seat is not too far from the pedals
- your knee should be slightly flexed when the foot presses the pedal to the floor
- have the back rest upright so that your arms are not straining to reach the steering wheel. Ensure your shoulders are relaxed
- ensure you are not gripping the steering wheel too tightly
- to get into the car, back onto the seat first and then bring in one leg at a time, turning on your tail
- avoid excessive twisting or bending of the spine
- to get out of the car, lift one leg at a time out onto the road, and then stand up.
Tips for household tasks
Laundry
- Avoid bending and retrieving wet clothes from the washing machine for the first four weeks.
- Use a trolley to carry loads to the clothes line.
- Avoid excessive bending and reaching when hanging the clothes by placing the clothes basket on a trolley or stool, and altering the height of the line.
- After neck surgery keep the line lower and the items light for six weeks.
Ironing
- Avoid standing and ironing for long periods. Start with short bursts (e.g. five to 10 minutes) after about two to three weeks following surgery.
- Place your ironing basket on a chair to avoid the need to repetitively bend.
- You many place one foot on a low footstool while standing.
- Ensure the ironing board is at waist height, so that your shoulders are relaxed and your spine is straight.
Cleaning
- Avoid activities that involve repetitive bending or twisting for the first four weeks. For example, vacuuming, sweeping, and scrubbing bathrooms. When you commence these activities, clean small areas at a time with adequate rest in between tasks.
- Avoid cleaning high up in cupboards on walls and ceilings for six weeks following neck surgery.
- Use long handled tools and upright vacuum cleaners.
- Use shorter strokes, bend knees and tighten your abdomen.
- Avoid twising by changing direction with your feet.
- Always face the area being cleaned.
Storage
- Arrange your cupboards so that items that are used most regularly are at waist height, those used less frequently are between knee and shoulder height, and those items used rarely are stored at the highest and lowest points. Store heavier items at the bottom, and lighter ones at the top of shelving. This will help to minimise the amount of bending you need to do.
Shopping
- You will need to organise some assistance with your shopping for the first four weeks, due to your lifting restrictions.
- Do not push a supermarket trolley or lift groceries in or out of the car for four weeks. You may walk around the shop without lifting. When you do start using a trolley, ensure that the wheels move easily, and that you keep your spine straight when turning corners.
Cooking
- On discharge, you may cook light meals.
- You may need to organise assistance for meals requiring more preparation.
- Organise the kitchen to negate the need to bend and reach over your head. See the section on storage for tips on how to organise kitchen cupboards.
- Try to work at bench height.
- Avoid cutting pumpkins or lifting large pans full of water.
Bathing
- You will usually be able to shower independently before leaving hospital.
- At home you may stand or place a chair in the shower and sit, if your balance is impaired.
- Do not have a bath for two to four weeks, as getting in and out of the bath can strain your back.
- Do not pick up soap from the floor if you cannot keep your back straight and bend your knees to do so. Use "soap-on-a-rope" or shower gel if you are concerned.
- You may have difficulty washing your hair after neck surgery or the insertion of a stimulator. Take it slowly and avoid the prolonged use of hairdryers and straighteners.
Sexual activity
- It is recommended that you do not engage in sexual activity for the first two to four weeks after your operation. Ensure that you communicate with your partner positions or actions that cause any spinal discomfort.
- Take a more passive role initially. You may be more comfortable lying on your back or on your side.
- Try to keep your spine straight and avoid pelvic thrust.
Tips for returning to sport
Depending on the type of surgery you have had and your specific pathology it may be possible for you to return to your chosen sport. As a general rule, a graduated return to sport may be considered after three months, if an appropriate exercise program has been undertaken first. It is best to discuss your specific case, as well as your goals, with your physiotherapist. They will be able to offer advice and tailor your exercise program to your specific needs.
Physiotherapy follow up
Continue with your exercises after discharge from hospital. Approximately two to three weeks after discharge, make an appointment with a physiotherapist so the exercises may be upgraded and you can be taught how to start returning to normal functional activities safely. If you are unsure about this process, please speak to your surgeon. Your rehabilitation after surgery is a crucial part of the journey to ensure recovery. It is recommended that you see a physiotherapist with access to real-time ultrasound to monitor activity of abdominal and spinal muscles and who has an exercise based practice (e.g. a Pilates studio). Your exercise program should be graded and specific to your case.
Physiotherapy goals
- To optimise muscle imbalances, function and endurance.
- To strengthen postural (core stability) muscles.
- To improve function at home, work and at leisure.
- To teach self management strategies.
Physiotherapy techniques
- Evidence suggests an active or exercise based approach is the best
- Specific therapeutic exercises are graduated, specific to your individual case and safe to perform
- Identify muscle irregularities
- Teach strategies to improve function
- Correct and teach correct movement patterns
- Joint mobilisations Rebalancing of the lower spine/pelvis and upper spine/shoulder girdle using land based exercise
- Hydrotherapy may be of value but not in isolation
- Occasionally passive treatments, e.g. Acupuncture, soft tissue release (massage), heat/electrotherapy and taping for biofeedback may be of value but not in isolation.
Remember that recovery from spine surgery takes time, and therefore a lot of patience. Increase your activity levels gradually. Use the information in this brochure as a guide only. Everyone's case is different. If you have any concerns about how best to care for your back and recover optimally, please discuss this with your physiotherapist.
Although this is a postoperative brochure, some patients may read this brochure preoperatively.
How can I best prepare for surgery?
Optimising your preoperative fitness and general strength and having an understanding of your spine, your procedure and the post operative period will improve your experience, functional outcome and overall quality of life post surgery.
Read this brochure to understand what modifications and restrictions will apply. These tips are appropriate to you pre operatively as well.
Be fit for surgery
- Lose weight if you are > 25 BMI (see how to calculate below) Even one to two kilograms will improve your ability to move in bed post operatively.
- Maintain cardiovascular endurance, e.g. walking, swimming, cycling on stationary bike or aqua exercises.
- Avoid/manage constipation prior to admission.
- Cease smoking, or at least cut down the number of
- cigarettes you smoke.
- Avoid exposing yourself to colds and the "flu". Wash your hands frequently and before each meal.
- If you have been seeing a physiotherapist preoperatively you may have been given an exercise program. Continue exercises that are pain free until surgery. A preoperative visit to a physiotherapist will teach you:
- how to move in bed postoperatively
- how to correctly activate and control the stabilising muscles of the spine. Learning this preoperatively will assist you in the postoperative phase. It is recommended that your physiotherapist has access to a real-time ultrasound to enhance the teaching
- how to start addressing muscle imbalances and lack of muscle control.
Calculating BMI is difficult. There are many calculators available on the internet. Just search ‘BMI calculator’ and enter your weight and height.
Or if you are mathematically minded, divide weight (in kilograms) by the square of your height (in meters).
Travelling to hospital
What to bring:
- Satin pyjamas or boxers, which allow for easy rolling and sitting in bed without lifting the pelvis as much—important for both back and neck surgery.
- Your usual pillow especially if it is an ergonomic one.
- Your usual walking aid especially wheeled walkers or frames (if you have one).
- If you are over 70 or your walking is impaired, borrow a walking stick or frame from a friend or relative that you may use in the early period if required.
Mater Private Hospital Brisbane
301 Vulture Street, South Brisbane Q 4101
Telephone: 07 3163 2590
© 2011 Mater Misericordiae Ltd. ACN 096 708 922.
Mater acknowledges consumer consultation in the development of this patient information.
Mater Doc Num: PI-CLN-450024
Last modified 09/8/2017.
Consumers were consulted in the development of this patient information.
Last consumer engagement date: 19/1/2014
For further translated health information, you can visit healthtranslations.vic.gov.au/ supported by the Victorian Department of Health and Human Services that offers a range of patient information in multiple languages.