Women’s health—chronic pelvic pain
What is chronic pelvic pain?
Chronic pelvic pain (CPP) is pelvic pain that that lasts for more than six months.
How common is CPP?
Chronic pelvic pain affects nearly 15 per cent (one in seven) of all women of reproductive age.
What does CPP do?
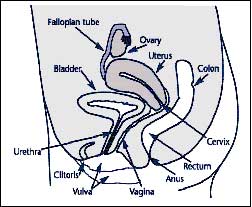 There are a number of initial events that may result in the development of CPP, such as endometriosis or infections. While pain usually indicates specific injury to some part of the body, CPP is very different. Often, the initial problem is addressed or lessened, but the pain persists because of changes in the nerves, muscles or other tissues. For instance, you often feel muscles tense when you have been injured around the area of trauma. Similarly, local disturbances can occur in the pelvis, affecting the bowel, bladder, muscles, connective tissue and nerves in the pelvis. Often these secondary factors become the main problem, overshadowing the original problem which may now be gone.
There are a number of initial events that may result in the development of CPP, such as endometriosis or infections. While pain usually indicates specific injury to some part of the body, CPP is very different. Often, the initial problem is addressed or lessened, but the pain persists because of changes in the nerves, muscles or other tissues. For instance, you often feel muscles tense when you have been injured around the area of trauma. Similarly, local disturbances can occur in the pelvis, affecting the bowel, bladder, muscles, connective tissue and nerves in the pelvis. Often these secondary factors become the main problem, overshadowing the original problem which may now be gone.
As this long term, unrelenting pain continues even the strongest person’s defences may break down, resulting in emotional and behavioural changes. By the time the pain becomes chronic, multiple systems—rather than a single problem—are involved in the pain process. The exact contribution of each pain factor to the total amount of your pain will need to be assessed.
What are the symptoms?
The symptoms of CPP are variable and do not always correspond to the severity of disease. Symptoms may include pain with periods, ovulation, during intercourse, when passing urine or opening bowels or lower back pain.
How is CPP diagnosed?
At the present time there is no simple test (such as a blood test) for CPP. Obviously, if the original source of injury remains, pain will continue. Much of the initial assessment will be focused on finding out whether this is the case and to determine any secondary factors. This will involve some careful questioning and an examination. Information may be sought from your previous health care providers and further tests ordered. You may be required to complete a “pain diary”. Such extensive assessment may be performed over a number of consultations and will often require the input of a number of specialists and practitioners.
Part of the assessment may involve keyhole surgery (laparoscopy) and obtaining a tissue sample (a biopsy). This is usually a day procedure under a general anaesthetic and some treatment may be undertaken at the same time.
What are the treatment options?
It is important to realise that your CPP has evolved over a long period of time and treatment may also be a long term process. Multiple interrelated problems are likely, and several treatments will probably be required. The approach to CPP will usually involve gynaecologists, pain physicians, occupational and physiotherapists, psychologists and other specialties. The initial cause of your problem (although important to identify and treat) may become a minor issue, while other factors become more important. All aspects of your condition must be treated, rather than just the ones you or your prior physicians thought to be most important.
Treatment options
 Surgery—a number of causes of CPP are amenable to surgical therapy, with a varying degree of success, although in established CPP no single surgical intervention is likely to result in a cure.
Surgery—a number of causes of CPP are amenable to surgical therapy, with a varying degree of success, although in established CPP no single surgical intervention is likely to result in a cure.
Drug therapy—drug treatment may focus on pain control and dealing with the secondary factors. These include medications used to treat pain (analgesics), depression (antidepressants) or seizures (anti-epileptics). Some forms of therapy may require injections or topical applications. As some of these medications have a potential for abuse, lost or stolen scripts will not be replaced and refills will not be issued. If it is discovered that you are obtaining additional medications, particularly opiates, through another physician without discussion and permission, you may be discharged from the clinic.
Physical therapy—occupational and physiotherapy will reduce the effects of inactivity on your body, help your body to function more normally, simplify your activities of daily living and teach relaxation and stress management techniques.
Psychology—CPP extracts both a physical and emotional toll and can result in dramatic changes to your lifestyle. Psychologists assist individuals to gain emotional confidence, increase control over their thoughts and feelings and gain a better understanding of the emotional contributors to pain.
Complementary therapy—many women find natural and complementary therapies helpful in the treatment of chronic pelvic pain. They can relieve the symptoms and may also assist the body to recover from drug or surgical treatments. Some women also find that natural and alternative therapies provide them with a sense of control. These therapies include dietary changes, exercise, herbal medicine, traditional Chinese medicine, aromatherapy, homeopathy, massage and yoga. Women interested in using complementary therapies should consult a qualified practitioner who can properly advise them on a course of treatment. It is also important that women disclose their use of any complementary therapies to their doctor, particularly if they are also undergoing medical treatment for CPP.
How effective is treatment?
Despite effective therapy there is no cure for CPP. Regardless of the type of treatment, it is estimated that one in five women will have recurrence of symptoms within five years.
Mater acknowledges consumer consultation in the development of this patient information.
Mater Doc Num: PI-CLN-430158
Last modified 09/8/2017.
Consumers were consulted in the development of this patient information.
Last consumer engagement date: 19/1/2014
For further translated health information, you can visit healthtranslations.vic.gov.au/ supported by the Victorian Department of Health and Human Services that offers a range of patient information in multiple languages.