Colposcopy results—what are the next steps?
After attending the colposcopy appointment, you often need to wait for test results before your doctors can tell you the next steps.
Sometimes, there is no need to do any tests and your doctor will inform you at the appointment that you can be returned to the care of your GP, usually for a repeat cervical screening test in 12 months’ time. We will also write to your referring GP and inform them of the plan.
If there are tests being performed, the results are usually available in one to two weeks and a doctor will call you and tell you the results over the phone. If we do not manage to speak to you, we will send you, and your referring GP, a letter with the results and follow up plan.
Most of the time, the follow up plan will include one of the following:
Repeat cervical screening in 12 months with your GP
-
This is usually if the results are reassuring and your doctors do not think there is any “high grade” disease that needs to be treated.
-
Most women after being seen in the colposcopy clinic will need to have a cervical screening test every 12 months until 2 consecutive tests are negative. Then most women will be able to have a test every five years.
Review of test results by gynaecology doctors and pathologist’s
This is not uncommon. The gynaecology doctors will review your case and tests results with the help of pathologists to decide on the best plan for management. We will phone you following this meeting and let you know what to do next.
Repeat colposcopy in six months
- Not everyone who has an abnormality in their cervix needs to have treatment. Often it is suitable to wait a short period of time, such as 6 months, to see if the condition improves on its own.
- If this is suitable in your case, your doctors will inform you in the follow up phone call
Have a procedure to remove the abnormal area from your cervix
-
This is usually done if there is “high grade” disease or a concern you could have a pre-cancerous lesion on your cervix.
-
There are two common types of excisions; a LLETZ (large loop excision of the transformation zone) and a cone biopsy which are explained below.
LLETZ and cone biopsy of the cervix
What is a LLETZ?
A LLETZ is a procedure to remove a small segment of the cervix (the lower part of your womb or uterus).
What is a cone biopsy?
A cone biopsy is a less common surgical procedure where a cone-shaped or cylinder-shaped piece of the cervix is removed.
Why are they performed?
These procedures are performed for the diagnosis and treatment of pre-cancerous cells of the cervix. You should have a clear understanding of your reason for this surgery—if not, please ask your doctor.
What are the alternatives?
A LLETZ or cone biopsy procedure is recommended in order to treat pre-cancer cells. If you chose not to undergo treatment, there is a risk that these changes would progress to cancer over some years. If you did not have treatment it would be essential for you to have ongoing close follow-up in the colposcopy clinic.
How are they performed?
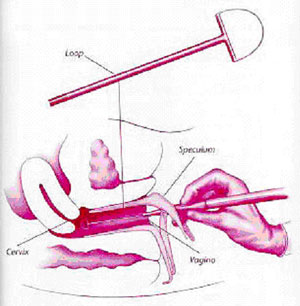 The procedure is usually performed under a local anaesthetic. The cervix is examined using a special microscope called a colposcope (in the same way as you were examined in the Gynaecology Clinic).
The procedure is usually performed under a local anaesthetic. The cervix is examined using a special microscope called a colposcope (in the same way as you were examined in the Gynaecology Clinic).
For LLETZ, a fine wire loop charged with electricity is used to shave away the abnormal tissue from the cervix. Because the procedure is so exact, and the loop very thin, very little damage is done to the tissue surrounding the area that needs to be removed. The procedure allows for the blood vessels surrounding the area to be sealed.
A cone biopsy may be performed under a local or general anaesthetic. The abnormal cells are often cut out with a scalpel. Dissolvable sutures are used to stop the bleeding.
Both procedures take approximately fifteen minutes.
What are the risks of undergoing this procedure?
Although the risks associated with a LLETZ procedure or a cone biopsy are low, you should be aware that every surgical procedure has some risk.
There are some specific risks to be aware of in relation to this operation:
- Excessive bleeding from the cervix, which may need blood transfusion or further surgery, either initially or within weeks of the procedure.
- Infection may be introduced into the cervix, uterus, tubes or abdomen. This may require treatment with antibiotics.
- Sometimes not all of the abnormal tissue is completely removed, requiring further surgery.
- Uncommonly, the cervix may be weakened by this procedure resulting in a slight increase in the future pregnancy risk of a late miscarriage or preterm birth.
- Rarely the cervix may be damaged and narrowed leading to painful periods, difficulty in performing adequate pap smears, or problems in the progress of a future labour.
What should I do before the procedure?
- You should expect a blood-stained vaginal discharge for several days after the procedure, which should settle within 1 to 2 weeks. A clear discharge may persist for up to 6 weeks.
- Follow up appointments are very important to ensure that all of the abnormal cells have been removed.
After discharge from hospital, you should:
- use sanitary pads (not tampons) if required
- shower in preference to having a bath.
You should not have sexual intercourse for 4 weeks.
What if I have any problems?
You should seek medical attention if you experience:
- a fever
- are feeling unwell
- offensive vaginal discharge or heavy bleeding
- severe pain.
Please contact our Gynaecology Case Manager or attend Mater’s Emergency Department if you require urgent attention.
© 2020 Mater Misericordiae Ltd. ACN 096 708 922
Mater acknowledges consumer consultation in the development of this patient information.
Mater Doc Num: PI-CLN-430015
Last modified 24/6/2020.
Consumers were consulted in the development of this patient information.
Last consumer engagement date: 22/6/2020
For further translated health information, you can visit healthtranslations.vic.gov.au/ supported by the Victorian Department of Health and Human Services that offers a range of patient information in multiple languages.