Appendectomy
 What is appendicitis?
What is appendicitis?
Appendicitis is inflammation of the appendix. It can be caused by an infection or blockage of the appendix. With a blockage, the appendix can become swollen and easily infected by bacteria.
Treatment
Treatment for appendicitis involves an operation to remove the appendix completely. The surgical team will discuss treatment options and factors involved with you, relevant to your child’s particular circumstances, as well as anyrisks associated with the treatment as part of the informed consent process. The operation may be performed through a single incision over the appendix or by laparoscopy (keyhole) surgery.
About one in five children who have an appendectomy actually have another cause for their pain. However, this has to be balanced against the risk of the appendix rupturing if the operation is delayed.
Admission phase
On admission the staff will show you to your child’s room in the ward. The admitting nurse will introduce themselves, show you around the ward and explain the available facilities. We will provide a bed for one parent if you wish to stay with your child overnight. Prior to theatre, you will be required to sign a medical consent form as part of the consent process. Your admitting nurse will apply an armband to your child which will stay on for the duration of their admission. They will also ask about your child’s medical/surgical history and any particular needs your child may have while in hospital.
Discharge planning
Your child can expect to stay in hospital for two days for a simple procedure, four days for a complex procedure, or until they have met the expected recovery outcomes. To prepare for your child’s discharge we must discuss what support and potential needs your child may have at home.
Tests and procedures
Any blood tests, x-rays or other tests ordered by your child’s doctor will be organised during the course of their stay.
Consultations
Your child may be seen by an anaesthetist prior to going to theatre. The doctor may also see you or your child again.
Mobility/hygiene/toileting
Before the operation your child is free to move about the ward. Please remain in the ward area at this time, in case your child’s nurse or doctor needs to speak with you. Your child may have a shower or bath before the operation and may walk to the toilet with assistance if required.
Medication
Please speak to your child’s nurse if you have any concerns about your child’s pain.
Nutrition
Your child cannot consume any food for six hours before the operation. This is called fasting. Depending on the circumstances, your child may be allowed to drink fluids—please check with your nurse or doctor if you are unsure.
Teaching/emotional support/ discharge planning
Today will be a day filled with new experiences. Please speak to your child’s nurse/surgeon/social worker or anaesthetist if you have any questions.
Your child’s nurse will discuss any needs they may have once at home prior to discharge. The expected date for discharge will be discussed with you. Please plan ahead where possible. On occasions, information will be provided about ongoing wound care treatment and/or Intravenous (IV) drip antibiotics.
Surgery phase
Before the operation
Your child will be seen and assessed by an anaesthetist, who may order some medications (pre-meds) for your child to have prior to theatre. Your child may have some anaesthetic (numbing cream) applied to the back of their hands, as they will have an IV to receive fluids and medications to keep them comfortable.
Prior to your child’s transfer to theatre, their nurse will complete a pre-operative check list. Your child will go to theatre either on a bed or in a wheelchair. They will stay in the recovery room following the operation while they wake up from the anaesthetic. If you are in the waiting room, the recovery nurse will call for you once your child is awake, to be with your child.
Following the operation
Your nurse will take frequent observations of your child’s vital signs (including pulse and breathing rate) and dressings for several hours after their operation.
As your child progresses through their recovery, these observations become less frequent, but remain regular while they are in hospital.
Immediately following surgery your child will be resting in bed. For safety reasons they are not to get out of bed without the assistance of a nurse. If your child has pain or has nausea, please notify us immediately, as there are medications available to ease this. Effective management of pain and nausea is vital to your child’s recovery and their ability to move, cough and achieve their recovery milestones. Your child will have an IV to maintain their fluid intake. The drip will be removed once your child is tolerating adequate amounts of oral fluids and IV medications are no longer required.
Your child will usually have three small dressings (laparoscopic procedure) or one larger dressing (single incision) on their abdomen. They may also have oxygen via a mask while they are waking up from the anaesthetic.
A physiotherapist may visit your child, if they had a pre-existing respiratory condition, to explain some breathing exercises that will assist their recovery.
Your child’s nurse is available to help them wash/shower after the operation if required. Please ask for assistance at any time.
Following surgery your child can have small amounts of water, increasing to free fluids and diet as tolerated, or as per your doctor’s instructions.
Your child may walk to the toilet with the nurse’s approval. Please ask if you require assistance.
Discharge planning
Any discharge needs that were raised and identified on admission will be discussed and necessary arrangements put in place. Your child’s planned discharge time is 10 am. Please ensure transport has been arranged for this time.
Day one after surgery
This is the expected day of discharge for children who have had a simple procedure and met their recovery milestones.
Consultation
Your child’s doctor will visit and discuss the operation with you.
Mobility
Your child is free to gently move around (as able), or with assistance if required. In the interest of your child’s safety please check with your nurse first.
Hygiene/toileting
Your child may have a shower or wash today with assistance as required. Your child may walk to the toilet with assistance. Please check with their nurse first.
Nutrition
Your child is able to eat and drink today as per the doctor’s instructions (please check with their nurse).
Observations/treatments
Your child’s nurse will continue to take regular observations of your child’s temperature, pulse, and dressings during the day. If your child’s appendectomy procedure was complex, your child may have drains in place, which collect wound drainage and assist in the healing process. The nurses will monitor this and the doctor will indicate when they can be removed.
Medications
The intravenous fluids will continue until your child is tolerating adequate amounts of fluids and the IV medications have ceased. Effective management of pain is important in your child’s recovery. Your child is likely to withhold coughing and movement if they are in pain. If your child has any pain or nausea please notify us immediately, as we can administer medications to alleviate this.
Discharge planning
If your child’s surgery was not complex and your child has met the necessary recovery milestones for discharge they can go home with their doctor’s approval.
Day two after surgery
Consultation
The doctor will visit your child today.
Mobility
Your child may gently walk around the ward (as able) with the approval of their nurse.
Hygiene
Your child may have a shower or a wash today (with assistance if required).
Toileting
Your child may walk to the toilet (assistance can be provided if required). Please let us know if your child has passed wind and/or had a bowel movement.
Nutrition
Your child may eat and drink as tolerated and/or as their doctor’s instructions (please check with your nurse).
Observations
Your child’s observations will continue to be taken and dressings/drains checked.
Medications
Your child may still experience some level of pain/discomfort, this is normal following surgery. While in hospital your child will receive pain relieving medication via their IV drip or medicine.
Treatments
The dressing/s will be changed only if required or as ordered by the doctor. Please check with your child’s nurse. Any drains your child has may be removed today as per the doctor’s instructions.
Teaching and emotional support
If you have any questions relating to your child’s surgery, recovery and care at home please ask their doctor/nurse/social worker.
Discharge planning
Any discharge requirements identified will be discussed and necessary arrangements put in place. Your child may be able to go home today if they have met the necessary recovery milestones (and with their doctor’s approval).
Day three after surgery
This is the expected day of discharge for children who have had a complex procedure and met their recovery milestones.
Consultation
The doctor will visit your child before they are discharged.
Mobility
Your child may walk around the ward.
Hygiene
Your child may have a shower or a wash. Assistance will be given if required.
Nutrition
Your child may eat and drink as tolerated.
Toileting
Your child may walk to the toilet. Please advise if your child is passing wind/has had a bowel movement.
Observations
Your child’s observations will be taken before discharge and dressings checked.
Medications
Your child may still experience some level of pain/discomfort, this is normal following surgery. Please discuss this with your nurse or doctor before you go home.
Treatments
The dressings may start to lift and may come off. You do not need to replace the dressings once they have fallen off.
Teaching and emotional support
If you have any questions relating to your child’s surgery, recovery and care at home please speak to your doctor/nurse/social worker.
Discharge planning
Prior to discharge, we would expect that:
- your child will be able to maintain an adequate oral intake
- your child’s wound will be free from infection
- your child’s pain will be controlled with oral analgesia (medicine).
If your child has met the necessary recovery milestones for discharge they can go home with your doctor’s approval.
After your child is discharged home
An appendectomy is a surgical procedure. It may take your child a few weeks to regain their usual activities.
At home, please:
- ensure your child maintains an adequate oral (in particular fluid) intake
- check your child’s wounds and ensure they are healing well—not red, warm to touch and no ooze.
The dressings are water proof so your child is free to shower/bathe. Your child may have some pain and discomfort at home.
Please continue to administer medicine for pain relief as required as instructed by your doctor.
Seek medical advice
If you notice any new wound discharge or bleeding at the wound site/s
- the wound becomes swollen, painful, red or warm to touch
- your child develops a fever (temperature higher than 37.5° C)
- there is a dramatic increase in your child’s pain
- your child is unable to maintain oral fluids and/or has nausea, vomiting or change in bowel patterns (e.g. constipation).
Please bring this information with you to any follow-up appointments your child may have, as it will assist their healthcare practitioner in knowing what care has been provided at Mater Children’s Private Brisbane.
How to seek urgent medical advice
To ensure your child receives the best possible care in an emergency, you should call 000 or go to your closest hospital that treats children.
If you have any concerns or questions please contact your doctor.
Home care phase
Mater Home Care Program
On occasion, a community nursing referral will be required where ongoing wound care treatment and/or IV antibiotics need to be administered at home. We will organise this for you based on your child’s recovery and individual discharge needs.
The nursing service works in partnership with Mater Health Services to provide care in the comfort of your home. The service ensures that:
- your child’s pain is managed on oral medications (tablets/medicine)
- your child’s wound is monitored and observed to be healing (as per their doctor’s instructions)
- your child is maintaining adequate oral intake
- your child is returning to usual daily activities based on age/ developmental status
- your concerns and expectations have been discussed.
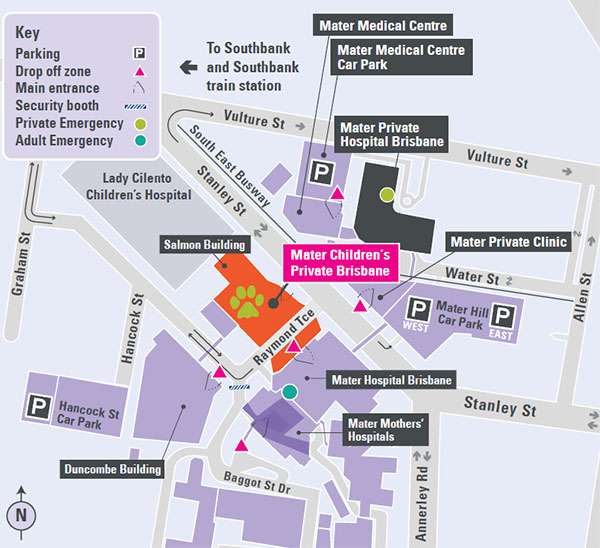
Contact Mater Children’s Private Brisbane
Salmon Building
Raymond Terrace
South Brisbane QLD 4101
Telephone: 07 3163 8111
Mater acknowledges consumer consultation in the development of this patient information.
Mater Doc Num: PI-CLN-470003
Last modified 09/8/2017.
Consumers were consulted in the development of this patient information.
Last consumer engagement date: 07/5/2015
For further translated health information, you can visit healthtranslations.vic.gov.au/ supported by the Victorian Department of Health and Human Services that offers a range of patient information in multiple languages.