Wide Excision and Breast Cancer Information
Mater Private Hospital Brisbane
The largest of Mater Health Services' private facilities, Mater Private Hospital Brisbane is a flagship for the level of care and facilities our organisation strives to provide.
The tertiary, acute facility is built on a foundation of clinical excellence and a commitment to safe, compassionate care, that is:
- quality focused
- technologically advanced
- customised to patients' needs and lifestyle.
Mater Private Hospital Brisbane is an outstanding health care provider with a total of 323 patient beds, 10 operating theatres, a 24-hour private emergency service, preadmission clinic, CardioVascular Unit, Intensive Care and Coronary Care Units, Breast Cancer Centre and Day Procedure Unit.
All rooms and facilities are designed to offer comfort and privacy, complete with a range of modern, air-conditioned accommodation.
While in hospital, patients also have access to allied health (e.g. dietitians, physiotherapists), pharmacy, hairdressing and chaplaincy services.
For more information about Mater Private Hospital Brisbane, please phone 07 3163 1111.
Visiting hours
8 am to 8 pm (patient rest period —1.30 pm to 3.30 pm)
Our Mission
In the spirit of the Sisters of Mercy, Mater Health Services offers compassionate service to the sick and needy, promotes an holistic approach to health care in response to changing community needs and fosters high standards in health-related education and research.
Following the example of Christ the Healer, we commit ourselves to offering these services to all without discrimination.
Our Values
Mercy: the spirit of responding to one another
Dignity: the spirit of humanity, respecting the worth of each person
Care: the spirit of compassion
Commitment: the spirit of integrity
Quality: the spirit of professionalism
At Mater Private Hospital Brisbane, we acknowledge that having an operation can be a very stressful experience. In keeping with our Mission to offer compassionate, quality care that promotes dignity whilst responding to patients' needs, this booklet aims to alleviate some of your concerns. It explains the general day to day events that may occur during your visit and what you may expect when you are discharged from hospital.
It is, however, only a guideline as each person may require differing treatments.
If you have any questions about your treatment, please speak to your doctor or the nurse caring for you.
Our breast care nurses are available to provide support to you during your hospitalisation and following your discharge. They can be contacted at Mater Private Breast Cancer Centre, from Monday to Friday between 9 am and 4.30 pm on 07 3163 1166.
Our pastoral care team also offers a caring support network to all patients. The dedicated members of this team are available at your request.
Our expectations
We expect that you will stay in hospital for between one to three days, or until:
- you are able to maintain an adequate oral intake
- you understand how to manage your wound and drain (if applicable)
- your pain is controlled with oral analgesia (pain medication)
- you are mobilising to the same level as you were prior to your admission
- you have an understanding of your ongoing exercise program and activity precautions.
Preadmission clinic
Mater Private Hospital Brisbane provides a preadmission service. You will receive this service in any of the following ways:
- from the specialty clinic to the preadmission clinic
- at the preadmission clinic
- via a phone call.
The preadmission service gathers information, initiates investigations to prepare you for your surgery, provides information regarding your specific operation and identifies your discharge needs.
Day of admission/surgery
Before coming to hospital please ensure that you have:
- had nothing to eat or drink as per the instructions given to you by the preadmission clinic or your doctor
- showered, shaved under your arm and dressed in clean clothes. No skin products are to be used following your shower. (e.g. deodorant, perfume, body lotion, powder, make up)
- left your valuables at home. You may wear your wedding band only
- brought the following with you:
- test results
- X-rays
- operation consent form
- medications in their labelled containers or packets.
- If your surgeon has arranged for any preoperative procedures such as wire localisation or sentinel node mapping you will be admitted early to allow time for results to be available before your surgery. These procedures will occur in the radiology departments. No visitors are permitted in the departments; however relatives are welcome to wait in Chloe's Coffee Shop, or the lounge area on level 6, Mater Private Hospital, Brisbane. Nursing staff will contact your relatives as soon as you return to the welcome lounge.
- If you are undergoing any preoperative procedures we recommend bringing along a book or magazine as you may need to wait several hours before your surgery.
On your arrival to the hospital please report to the reception desk on level 6 of the hospital where you will be directed to the welcome lounge/Day Procedure Unit. Only one relative/visitor is permitted within the clinical areas of the welcome lounge.
Our welcome lounge staff will:
- apply an identification band
- complete your nursing assessment form
- record your temperature, pulse, blood pressure and weight
- ask you to change into a theatre gown and paper pants
- apply anti-embolic stockings. These assist with blood flow through your legs and decrease the risk of blood clot formation while you have decreased mobility
- take details of ny family member who would like to speak to your surgeon after your operation (preferably mobile phone number)
- complete your preoperative checklist.
You may walk around as much as you like, but we ask that you do not leave the welcome lounge.
Your surgeon may visit with you prior to your surgery, either in the welcome lounge/day unit or in the preoperative holding area. You will be transferred to the operating theatre on a wheelchair or on your bed if you have received a premedication. Your luggage will be delivered to the ward where it will be stored in a locked room until after you have returned from theatre.
After your surgery
- Immediately following your surgery you will be transferred to the recovery room where you will be observed closely until you begin to awaken.
- It is common to need oxygen which will be given via a face mask.
- When you have recovered sufficiently from the anaesthetic you will be returned to your room in the post-operative ward. The nurses will record your vital signs—pulse, respiration rate, temperature, blood pressure— and check your wound and drain regularly.
- Your doctor will order pain relief and anti-nausea medications for you. Please tell your nurse if you have any pain or nausea, so these symptoms can be managed.
- Following your operation you will be offered ice to suck or water to sip. After a few hours you can begin to eat and drink as you are able. Intravenous fluids (a drip) will be administered until you are able to eat and drink.
- Initially, you may have a drain in place under your arm where the lymph nodes have been removed.
- When you are feeling more awake your nurse will assist you to have a wash and change into your own bed clothes.
- Your physiotherapist or occupational therapist will visit the day following surgery to explain exercises that will help with your post-operative recovery.
- If you have undergone a sentinel node biopsy your skin colour, urine and bowel movements may have a bluish tinge. This is due to the blue dye that is used during the procedure.
- It is important that you begin your breathing and leg exercises. These help prevent complications such as chest infections and blood clots in your legs and should be carried out every hour that you are awake and while you are on bed rest.

Breathing exercises:
Take five long and slow deep breaths. Each breath should be deeper than the previous breath. Think about getting the air to the very bottom of your lungs.
Circulation exercises:
Firmly move your ankles up and down to stretch and contract your calf muscles.
Post-operative phase—Days one and two
Mobility
You will be able to mobilise as you desire. Nursing staff will assist you as required. It is important to move around in order to maintain good circulation and prevent complications. It is also advisable to plan a quiet afternoon and rest. We suggest you limit your visitors during this phase.
Hygiene
You may shower yourself or nursing staff will assist you as required.
Dressings
Your dressings will be removed when instructed by your surgeon. Once the dressings have been removed, wash your wound with soapy water and pat dry.
Drain care
If you are being discharged with the drain in place you will be shown the Early Discharge with Exudrain" DVD and given the accompanying booklet to read. You will be provided with contact numbers should you experience any problems with your drain.
Exercises
Please continue the exercises given to you by your physiotherapist or occupational therapist.
Observations
Your vital signs, wounds and drains will be checked regularly.
Elimination
Please let the nurse know if you have any changes in your elimination patterns (bowel and or bladder).
Consults
- Your surgeon will visit daily to discuss your progress and any ensuing results and treatments.
- One of our breast care nurses will visit you during your stay (Monday to Friday).
- The ward nurse manager will endeavour to visit you daily. This is to provide you with an opportunity to discuss any aspects of your care or voice concerns or complaints you may have regarding your hospital stay. Any concerns after hours can be directed to the shift team leader or after hours nurse coordinator. Your feedback is important to us.
Day of discharge
- Discharge time is 10 am.
- A discharge summary form will be provided and discussed with you.
- Your own medications will be returned to you and any new ones will be supplied.
- Your X-rays will be returned to you.
- Your post-operative appointment will be discussed with you.
What to expect after you return home
Pain management
You may require some mild pain relief for wound discomfort as ordered by your surgeon.
Wound management
Your wound may be slightly red, raised and you may have some bruising. This is part of the normal healing process. Up until three months following surgery, your wound may become thickened—this is known as scar tissue
Drain
If you have been discharged with your drain in place please follow the instructions given to you.
Exercises
Please continue the exercises given to you by your physiotherapist or occupational therapist. You can expect to have full shoulder movement by six weeks. If you have any problems with your range of movement, please contact the breast care nurse (on 07 3163 1166) or your surgeon.
Nutrition and rest
Maintaining a nutritious diet, adequate fluids, gentle exercise and rest will aid your recovery. You can increase your daily activity as you feel stronger. After a few days at home, start walking short distances (e.g. five to 10 minutes) twice a day.
It is important to notify your surgeon if:
- your wound becomes red or inflamed
- you notice any discharge from your wound
- you develop a fever (temperature above 38 degrees Celsius)
- you have pain that is not relieved by simple pain medication.
Breast cancer
The principles of breast cancer treatment are to:
- treat the breast in which the cancer has developed
- assess and treat the lymph nodes in the axilla
- treat the rest of the body if there is any significant risk that cancer cells may have spread.
Wide local excision/ lumpectomy
Breast conservation treatment is defined as the excision of the primary breast tumour and adjacent breast tissue (breast-conserving surgery), usually followed by radiotherapy.
A pathologist will analyse the breast tissue that has been removed. If the tumour extends near to the edge of this removed tissue, you may require another operation called a re-excision.
There can be a cosmetic deformity where the tumour has been removed. This can be a minor indentation and slight distortion of the nipple depending on the site of your excision.
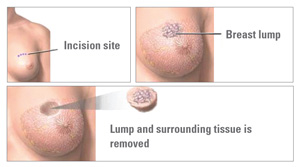
There is usually no need to change bra size following the removal of the tumour from your breast. After recovering from this operation, (approximately one month), the remaining breast tissue is treated with a course of radiotherapy.
About 80 per cent of breast cancers can be managed this way.
A mastectomy will not be performed if a breast conservation procedure such as a wide excision has been decided in consultation with your doctor. If a mastectomy is subsequently required it will be discussed in further consultations.
Mastectomy
Mastectomy is the removal of the breast tissue, including the nipple. Twenty percent of breast cancers will require mastectomy.
Mastectomy is recommended if:
- the tumour is in more than one part of the breast
- the tumour is large
- there is a strong desire not to have post operative radiotherapy
- post-operative radiotherapy would be inconvenient (e.g. if you live away from the east coast)
- mastectomy is your personal choice.
A breast reconstruction may take place at the time of mastectomy, or subsequently, following the surgery.
The lymphatic system
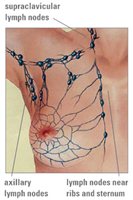
The lymphatic system is a network of glands that are connected by tiny tubes called lymph vessels that carry lymph around the body and into the veins. Lymph is a yellow fluid full of cells called lymphocytes. Lymphocytes help fight disease and rid the body of waste products. The diagram to the right displays the lymph drainage of the breast.
Why are the lymph nodes removed?
Lymph nodes under the arm can be the first place that breast cancer spreads. The only way to determine if breast cancer has spread to the lymph nodes is to remove and analyse them. Lymph node removal is performed for individuals who have invasive breast cancer, whether they undergo breast conservation or mastectomy. Lymph node analysis is instrumental in determining your future treatment plan.
Sentinel lymph node biopsy
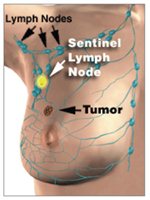
Sentinel lymph node biopsy maps the very first lymph node that would be encountered in the lymph node basin draining away from the breast cancer. The biopsy is performed under general anaesthetic by injecting blue dye around the tumour. The dye moves quickly into the lymph vessels and stains the sentinel nodes blue, allowing the surgeon to identify them. The dye stains the urine, faeces and drainage fluid blue or green for a day or so after surgery. It also stains the skin on the breast but this gradually fades over time.
Sentinel lymph node mapping may also be performed prior to your surgery by injecting a small amount of radioactive fluid (approximately five percent the dose of a bone scan) around the tumour. The first lymph node is then detected using a hand held Geiger counter. Your surgeon will provide you with information about this test.
Lymph node clearance (axillary dissection and axillary clearance)
If the breast cancer has already spread to the lymph nodes in the axilla (e.g.palpable or seen on ultrasound) a lymph node clearance of the axilla is recommended. This helps to control the cancer in the axilla and prevents further spread. Likewise, if the sentinel node contains cancer cells, further lymph nodes will need to be removed.
Within a week of surgery, provided that no further surgery is required, you will consult with a radiation oncologist and a medical oncologist to plan the next phase of your treatment.
Recovery
Most patients are sufficiently pain free, and able to return home within a day or two of surgery. If an axillary dissection has been performed a thin, plastic drain is inserted into the armpit where the lymph nodes were removed. This stays in place until the drainage is less than 50mls of fluid on two consecutive days, or less than 30mls on one day. Patients are able to go home with this drain in place although it is sometimes removed before discharge. The nursing staff will teach you how to manage the drain at home if you are discharged with your drain in place. They will also provide you with contact telephone numbers in case you require assistance after hours.
Emotional adjustment
Each woman reacts to breast surgery in her own way. There is no one way to cope with the diagnosis. You may feel temporarily anxious or insecure about the effects of the diagnosis on you, your partner and your family. We understand being diagnosed with cancer and the subsequent treatment is very stressful. Any surgical procedure consumes a great deal of physical and emotional energy. Increased fatigue, hospital confinement and temporary physical limitations may lead to feelings of nervousness, frustration, depression or even anger. Although these reactions are normal and temporary, they may distress you. Do not expect your emotional stress to resolve instantly. Speaking to someone close to you, with our breast care nurse, or one of our staff may help you to adjust physically and emotionally. Most women feel comfortable resuming their normal activities over time, although the length of time needed to adjust varies considerably between individuals.
Post-operative arm exercises/ physiotherapy
You will be visited by a physiotherapist or occupational therapist who will demonstrate exercises, discuss the care of your arm and early mobilisation of the shoulder and assist in regaining full range of movement of your arm. You will also be provided with a leaflet that will describe these exercises in further detail.
Side effects of surgery
Lymph node removal stretches a nerve in the armpit. This nerve may also be cut to allow for removal of the lymph glands. As a result, many women who undergo breast surgery will experience a degree of numbness on the inside of their arm. There will be some pain on moving the shoulder where the lymph nodes have been removed and occasionally limitation of movement due to scarring in the armpit, particularly in the early months after surgery.
Lymphatic fluid sometimes builds up under the wound after the removal of the armpit drain. This fluid is called seroma. If this becomes symptomatic, the fluid can be aspirated by your doctor to make you more comfortable.
Lymphoedema is a swelling of the arm and may develop in approximately five to 15 per cent of patients undergoing lymph node removal. The risk of lymphoedema can be reduced by avoiding the triggering factors that are outlined in the information provided to you. Staging investigations
Bone scans, chest X-rays and liver scans may also be requested by your doctor.
Treatment of the rest of the body
Adjuvant therapy
Additional treatment is often advised after surgery. This is called adjuvant therapy. It can take the form of radiotherapy for the breast or systemic therapy which treats the rest of the body. It varies from patient to patient but frequently involves combinations of hormones, chemotherapy or other medication.
Chemotherapy
Chemotherapy is a form of systemic treatment. If you require chemotherapy you will be referred to a medical oncologist. This treatment will be given at two or three week intervals for up to six months or longer. Chemotherapy education sessions are available and provide valuable information for you and your family.
Radiotherapy
Radiotherapy is a treatment that uses radiation to treat any remaining breast tissue cancer. A small dose is given and the procedure takes less than five minutes each working day for up to six weeks. Education sessions are available for you and your family at your treatment centre.
Herceptin
Apart from hormones and chemotherapy a sophisticated biological agent, Herceptin has been shown to be effective in preventing cancer recurrence in susceptible patients. Test results on your tumour will determine if you require this treatment. It is only indicated if you have a HER-2 positive tumour.
Hormone therapy—Tamoxifen/ Arimidex/Femara (oral medications)
Tamoxifen works by blocking the stimulating effect of oestrogen on breast cancer cells. Arimidex and Femara work by lowering oestrogen levels for post-menopausal women. Like chemotherapy, hormone therapy is a systemic treatment. These medications are usually taken for five years following surgery in cases where the cancer is sensitive to hormones.
| Follow-up period |
Frequency of follow-up visits |
| First year |
Three monthly |
| Second to fifth years |
Six monthly |
| Fifth year |
Yearly(you may be discharged back to breast screening or your local GP at this time) |
| Test |
| Mammogram and ultrasound |
Yearly |
Mater acknowledges consumer consultation in the development of this patient information.
Mater Doc Num: PI-CLN-440004
Last modified 09/8/2017.
Consumers were consulted in the development of this patient information.
Last consumer engagement date: 21/4/2011
For further translated health information, you can visit healthtranslations.vic.gov.au/ supported by the Victorian Department of Health and Human Services that offers a range of patient information in multiple languages.