Total hip replacement
Welcome
At Mater we understand that being in hospital can be a very stressful experience. This information aims to alleviate some of your concerns in keeping with our Mission to offer compassionate, quality care that promotes dignity while responding to patients’ needs. It explains briefly the events that may occur during your visit and the things to expect when you are discharged from the hospital.
It is, however, only a guideline as each person may require differing treatments.
If you have any questions about your treatment please ask your doctor or nurse.
Our pastoral care team offers a caring support network to all patients. The dedicated members of this team will visit you during your stay and are available at your request to discuss any anxieties or problems that you may have.
What is a total hip replacement?
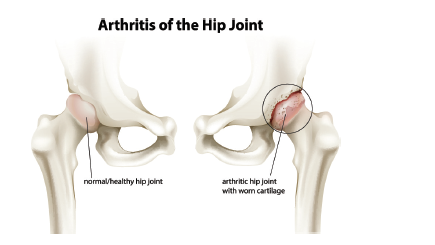
The hip joint is a type of ball and socket joint. The ball is formed by the head of the thigh bone (femur) and the socket is formed by part of the pelvis (acetabulum).
Usually the surfaces of the bones are covered with a smooth coating (articular cartilage). This allows smooth, pain free movement in all directions.
When people have problems with their hip, the hip can be painful, stiff and have
trouble moving normally. Hip replacement is a treatment that can reduce hip pain
and improve the way the hip moves.
What happens during hip surgery
The damaged areas of the bone are removed and your doctor will replace your hip joint with a man-made hip joint called ‘prosthesis’. Prosthesis can be made out of plastic, metal or ceramic.
You have the opportunity to donate the bone that has been removed from your hip
to the Queensland Bone Bank. If you would like to donate your bone you will be asked to complete a form and have a blood test.
What things do I need to do to be ready for surgery?
You will have received instructions from your doctor and the pre-admission clinic.
The Clinical Nurse Consultant will call you three days from before your surgery to
ensure you are on track with your preparations for surgery.
Please follow those instructions and complete the 'My checklist to be ready for
surgery'.
Having your home prepared before you have your operation will make things easier
when you return home after your operation. To help you with this, an occupational
therapist from Mater at Home will organise a time with you to review your home
set-up. They will review the following:
- bed height
- chair height
- walkways (to be clear of furniture, loose mats or rugs, cords or leads)
- shower, bath and toilet access and safety
- kitchen layout (re-arranging kitchen cupboards may be necessary to avoid bending).
Preparing meals in advance and freezing them, or buying frozen dinners will help
make meal preparation easier when you return home. You will need to organise
family, friends or neighbours to help with the housework, shopping, driving or
providing light assistance with showering dressing and putting on and taking off the
stockings required to be worn for six weeks after your operation.
What can I expect after my operation?
Operation and recovery - Your operation will usually take between one to two hours.
You will then remain in the recovery area until you are awake
enough to return to the ward. This may take up to three hours.
Lines and drains - When you return to your ward you may still need oxygen, will
have IV lines for fluid and pain medication, one to two wound drains and you may have a catheter to help keep your bladder empty until you are able to manage getting up to go the
toilet. These will be removed gradually from Day 1 following your surgery. Your operated leg will be resting in a foam trough to keep it supported and protect it from movements that could harm the operated joint.
Diet - If you eat and drink normally straight after your operation it may cause you to feel sick. Eating and drinking small amounts slowly will help to prevent this. You should be eating and drinking normally by Day 1 following your operation.
Pain - It is normal to have some pain and discomfort after your surgery. However, it is important that your pain is controlled so you are able to cough, breathe deeply and do your exercises. Please let someone know about your pain so it can be treated and managed.
Infection control - Every effort will be made to prevent infection in your artificial joint. Hand hygiene is essential when recovering from this surgery. Please wash your hands regularly.
Do not disturb the dressing on you operation site.
Your doctor may order antibiotics to also help prevent infections.
Mobilising and exercising - Your physiotherapy will begin on the day of your operation and an
exercise program will be given to you by your physiotherapist. This program will continue when you go home.
Blood clot prevention - To help prevent blood clots forming in your legs (thromboembolism) your doctor may request that you wear a pair of white compression stockings as well as compression pumps after your surgery. If your doctor has ordered stockings they can be removed for your shower and put back on afterwards. You will need to wear the stockings for six weeks after your operation. Non-slip socks will also be provided. You can wear these or
appropriate footwear over your stockings. You will have bloodthinning medication which may continue when you go home. If your doctor orders this, your nurse will provide education for you or your carer to manage this when you go home.
Bowels - Bowel function can be affected by surgery and medication. To help your bowels return to normal function you may require bowel medication. Increasing your water intake and eating food high in fibre will also help your bowel function to return to normal. Including prunes and pear juice in your diet is recommended.
Precautions for your new hip - For three months after your operation there is a risk that your
new hip could dislocate in some positions. Dislocation is when the parts of your hip separate. To avoid dislocation you should adhere to the following precautions:
- avoid sitting in low chairs
- avoid squatting, jumping, running and high impact sports.
Follow your surgeons, advice and instructions.
Going home - Depending on your recovery, it is anticipated you will be discharged after day 3 following your surgery. We aim for discharge from the ward to be 10 am. You should have already organised your own transport home, help with meals, driving, domestic tasks, shopping and getting your compression stockings on. Make sure the people helping you are aware of your discharge.
What complications could occur?
Serious problems from a hip replacement are not common but can happen.
- During the hip replacement surgery a bone can break or nerves and blood vessels in the area can be damaged.
- Soon after surgery people can get an infection or blood clots in their legs.
- The new prosthesis sometimes pops out of place.
- Some years later the hip joint can become loose causing the prosthesis to pop out of place. It may become stiff or simply wear out.
Although doctors take their time to measure your leg length carefully sometimes the leg may end up slightly longer.
If you experience redness, pain or swelling in your limb, or shortness of breath, you must present to the Emergency Department immediately. These could be signs of a Deep Vein Thrombsis (DVT - blood clot in the leg vein ) or a Pulmonary Embolism (PE - blood clot in the lung).
What can I expect from my physiotherapist and occupational therapist?
You can contribute greatly to the success of your operation by following the
instructions of your health team. It is important to consider yourself as part of the team.
Physiotherapist - While you are in hospital your physiotherapist will give information on:
- deep breathing and circulation
- getting in and out of bed
- sitting
- walking
- going up and down stairs
- getting in and out of a car
- taking precautions with your new hip as advised by your doctor.
Occupational Therapist
Your occupational therapist will have assessed the best method for you to shower or bath in your home and will discuss with you dressing, lifting, carrying and gardening.
What will it be like down the track - getting back into life!
After three months you should be back to most of your usual activities. You may find that you can return to activities you haven’t been able to do for some time because of your hip pain. Make the most of these improvements by getting back to activities you enjoy. Please check with your doctor before resuming driving. Having prepared yourself well and participated actively in your treatment, you will be able to return quickly to a more active independent lifestyle.
Acknowledgements
Staff of Mater Hospital Brisbane
Allied Health and Mater at Home
The Royal Brisbane Hospital Orthopaedic Transitional Care Project
Sponsored by Queensland Health
A Guide to Total Hip Replacement
Mater Hospital Brisbane
Raymond Terrace, South Brisbane Q 4101
Telephone: 07 3163 8111

Acknowledgments
Staff of Mater Adult Hospital, South Brisbane
Domiciliary Acute Rehabilitation Team (DAART)
The Royal Brisbane Hospital Orthopaedic Transitional Care Project Sponsored by Queensland Health, A Guide to Total Hip Replacement
© 2013 Mater Misericordiae Ltd. ACN 096 708 922.
Mater acknowledges consumer consultation in the development of this patient information.
Mater Doc Num: PI-CLN-420037
Last modified 13/5/2019.
Consumers were consulted in the development of this patient information.
Last consumer engagement date: 11/8/2015
For further translated health information, you can visit healthtranslations.vic.gov.au/ supported by the Victorian Department of Health and Human Services that offers a range of patient information in multiple languages.