Understanding and managing acute pain
Managing pain after your operation
Some discomfort/pain after surgery is expected and your experience can be quite different from others having the same operation.
Good pain control is important to assist your recovery. Moving around, taking deep breaths and coughing helps prevent complications such as chest infections and blood clots.
The aim is for you to have only mild discomfort. Speak to your nurse if you require more pain relief before you become too uncomfortable, before walking or physiotherapy.
Assessing your pain
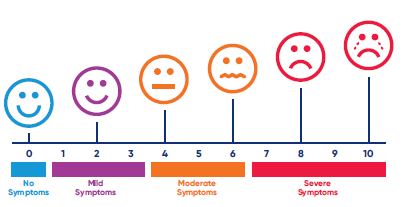
Nurses will ask you to score your pain using a scale of 0 to 10, with 0 meaning no pain and 10 being the worst pain you could imagine. You may also find it easier to use words such as mild, moderate or severe.
Treating your pain
Mild to moderate pain
Your physiotherapist will advise you on how to move in a way that is safe and to minimise discomfort. Simple techniques such as relaxation (deep breathing or meditation), diversional activities (reading, watching TV, colouring in, listening to music), massage or hot/ cold packs may be helpful.
Regular simple pain relief may be given to you by your nurses, for example:
- paracetamol (Panadol®, Panamax®)
- anti-inflammatory medicines such as ibuprofen, (Nurofen®), diclofenac (Voltaren®) OR celecoxib (Celebrex®).
If you remain uncomfortable, stronger medicines are available which you can ask for.
Severe pain
For severe pain, a group of medicines called opioids may be prescribed along with the regular simple pain relief. These include morphine, fentanyl or oxycodone, (Endone® or OxyNorm®) or other medications with similar acrtions such
as tramadol (Tramal®), tapentadol (Palexia®) and bupremorphine (Temgesic®) may also be used.
The nurses will need time to check these medicines as they are kept in a locked cupboard. Therefore, it is important to ask for these medicines if your pain is becoming severe or you are planning to mobilise.
Another way of managing severe pain is called ‘Patient Controlled Analgesia’ or PCA—the opioid medicine is in a locked pump attached to a ‘drip’ in your arm. If you have pain, you can self-administer a small dose of your pain medicine by pressing a button on the handset. Only you should press the button, as only you can determine how it makes you feel.
Sometimes local anaesthetics are used to temporarily numb a part of your body and can be used with, or without opioids to help your pain relief and can be administered in the following ways:
- Epidural—a catheter is placed into your back with medicines given through the catheter to block sensation and pain. The catheter may be left in place for up to three days.
- Spinal—medicines are given into your back and the pain relief can last for up to 24 hours.
- Regional—medicine is injected around the nerves under the skin. A catheter is sometimes left in place for up to three days.
- Local—injection of medicine into the area being operated on; pain relief can last several hours
If you have had an epidural, spinal, regional or patient controlled analgesia, you will be checked daily by the Acute Pain Service staff or your private anaesthetist/ surgeon. They will discuss the effectiveness of your pain relief and make changes as necessary.
When you are able to resume eating and drinking, and as you improve, they will change your intravenous pain medicine to tablets.
What about opioid-related side effects?
Our aim is to keep you as comfortable as possible with minimal side effects from medication.
Tell your nurse if you are feeling sick or vomiting, sleepy, itchy, unable to pass urine, constipated, or dizzy. Other side effectscan include a slowed breathing rate and confusion. If your alertness or coordination is affected, do not mobilise without assistance.
Going home
Your doctor will make a plan for your discharge pain relief. The pharmacist and nurse will discuss this plan with you, before you leave hospital.
Acute pain will get better as you heal. We expect you to gradually reduce and then stop the pain medication, as you recover. If your pain is not improving as expected, please see your general practitioner (GP). Your GP can also review your pain and your medication, then help you with this step-down process.
If you are continuing to take opioid medication after going home, you should not drive or operate heavy machinery.
Do not combine any other medicines, natural therapies or alcohol with the medications you are given to take home, unless you first discuss with your doctor or pharmacist. Please keep medications in a safe place away from children.
Any unused pain medications should be returned to your local pharmacy.
Breastfeeding and opioids
All medicines are passed into breast milk to some degree. The amount of medicine that passes to your baby depends on the drug, dose, how frequently you are taking the medicine and how often your baby is feeding.
Opioids reach maximum levels in breast milk, one to two hours after taking a dose. Minimise the amount of opioid passed to your baby through breast milk by taking your dose just before or just after breastfeeding.
The amount of opioid passed into your breast milk is considered minimal, especially within the first three days after birth. However, it is still important to monitor your baby for signs of unusual drowsiness and sleepiness, stomach upsets (especially diarrhoea) or any changes in feeding patterns e.g. not waking for a usual feed.
Be aware when handling your baby that opioid medication can affect your alertness and coordination. You may feel drowsy, dizzy and have slow reaction times, putting you at risk of falling, or the baby falling from your lap. If you feel these symptoms:
- place your baby in a safe place e.g. cot, do not mobilise and ask for assistance from midwifery staff, family and friends
- reduce the amount of opioid medication you are taking.
If you have any questions or concerns about taking opioids or any other medicines and breastfeeding speak to your midwife, doctor or pharmacist.
The Australian Breastfeeding Association also provides advice via 1800 686 268.
Mater acknowledges consumer consultation in the development of this patient information.
Mater Doc Num: PI-CLN-430062
Last modified 16/12/2019.
Consumers were consulted in the development of this patient information.
Last consumer engagement date: 02/9/2019
For further translated health information, you can visit healthtranslations.vic.gov.au/ supported by the Victorian Department of Health and Human Services that offers a range of patient information in multiple languages.