Hysterectomy
Mater Private Hospital Springfield
 Mater Health Services has a strong history, providing exceptional care to the Queensland community for more than 100 years. This tradition of care has been continued with the establishment of Mater Private Hospital Springfield.
Mater Health Services has a strong history, providing exceptional care to the Queensland community for more than 100 years. This tradition of care has been continued with the establishment of Mater Private Hospital Springfield.
Mater Private Hospital Springfield is an innovative, unique and contemporary hospital with a total of 80 beds, four digitally integrated operating theatres, a day surgery unit and a state-of-the-art cancer care centre featuring a linear accelerator and 15 medical oncology treatment bays.
Mater Private Hospital Springfield also offers a range of medical and surgical services including: General Medicine; Medical Oncology; Rehabilitation; Respiratory; Ear, Nose and Throat; Gastroenterology; General Surgery; Gynaecology; Ophthalmology; Oral and Maxillofacial; Orthopaedics; Plastics and Urology.
All rooms and facilities are equipped with the latest technology and have been designed with the family in mind, with a fold out bed in each room so family and friends can stay overnight. Integrated room controls allow patients to control temperature, blinds and lighting for optimal comfort.
Mater is committed to caring for the Greater Springfield community and as it continues to grow our services will grow with it.
For more information about Mater Private Hospital Springfield, please call 07 3098 3900.
Visiting hours
Mater Private Hospital Springfield is committed to providing family centred care and has no set visiting hours.
Our Mission
In the spirit of the Sisters of Mercy, Mater Health Services offers compassionate service to the sick and needy, promotes an holistic approach to health care in response to changing community needs and fosters high standards in health-related education and research.
Following the example of Christ the Healer, we commit ourselves to offering these services to all without discrimination.
Our Values
- Mercy—the spirit of responding to one another
- Dignity—the spirit of humanity, respecting the worth of each person
- Care—the spirit of compassion
- Commitment—the spirit of integrity
- Quality—the spirit of professionalism
At Mater Private Hospital Springfield, we acknowledge that having an operation can be a very stressful experience. In keeping with our Mission to offer compassionate, quality care that promotes dignity whilst responding to patients' needs, this booklet aims to alleviate some of your concerns. It explains the general day to day events that may occur during your visit and the things to expect when you are discharged from the Hospital.
It is, however, only a guideline as each person may require differing treatments.
If you have any questions about your treatment please speak to your doctor or nurse.
Our pastoral care team also offers a caring support network to all patients. The dedicated members of this team are available at your request.
Our expectations
We expect that you will stay in hospital for two to four days or until you have achieved the following:
- you are able to maintain an adequate oral intake
- you will be able to pass urine normally
- your pain is controlled with oral analgesia (pain medication)
- you are mobilising to the same level as you were prior to your admission
- your wound (if applicable) is healing well with no signs of infection.
Preadmission service
You should expect to be contacted approximately 48 to 72 hours before your planned admission by one of our hospital administration team who will confirm your personal details and provide you with an estimate of any excess or hospital expenses not covered by your private health insurance.
Additionally one of our preadmission team will contact you to talk about your procedure and complete a nursing assessment and health history interview. This allows you to ask any questions about your upcoming hospital stay and for our staff to ensure we have all relevant details required.
Day of admission/surgery
Before coming to hospital please ensure that you have:
- had nothing to eat or drink as per the instructions given to you by the preadmission clinic or your doctor
- showered and dressed in clean clothes. No skin products are to be used following your shower (e.g. deodorant, perfume, body lotion, powder, make up)
- left your valuables at home. You may wear your wedding band only.
- brought the following with you:
- your X-rays
- your operation consent form
- your medications in their labelled containers or packets.
On your arrival to the hospital please check in with our friendly front reception staff in the main foyer on level 2 of the hospital. When you check in staff will confirm your details, assist you to complete any required paperwork and direct you to the appropriate patient care area.
Our Nursing staff will:
- apply an identification band
- complete your nursing assessment form
- take your temperature, pulse, blood pressure and weight
- clip your vaginal or supra pubic area if required
- ask you to change into a theatre gown and paper pants
- apply anti-embolic stockings. These assist with blood flow through your legs and decrease the risk of blood clot formation while you have decreased mobility
- take details of any family member who would like to speak to the surgeon after the operation (preferably a mobile phone number)
- complete your preoperative checklist
You will be transferred to the operating theatre on a wheelchair or on your bed if you have received a premedication.
Your luggage will be delivered to the ward where it will be stored in a locked room until after you have returned from theatre.
After your surgery
- Immediately following your surgery you will be transferred to the recovery room where you will be observed closely until you are more awake.
- It is common to need oxygen which will be given via a face mask.
- When you have recovered sufficiently from the anaesthetic you will be returned to your room in the postoperative ward. The nurses will take vital signs—your pulse, respiration rate, temperature, blood pressure and check your wound (if applicable) and vaginal discharge regularly.
- If you have had a vaginal procedure you may have a vaginal pack in place which is usually removed the day after your surgery.
- A urinary catheter may be in place to drain urine from your bladder.
- You may have a drain in your abdomen close to your wound site.
- Your doctor will order pain relief and anti-nausea medications for you. Please tell your nurse if you have any pain or nausea, so these symptoms can be managed.
- Following your operation you will be offered ice to suck or water to sip. After a few hours you can begin to drink fluids as you are able. Intravenous fluids (a drip) will be administered until you are able to eat and drink.
- When you are feeling more awake your nurse will assist you to have a wash and change into your own bed clothes.
- If requested by your doctor, a physiotherapist will visit the day following surgery to explain exercises that will help with your postoperative recovery.
- It is important that you begin your breathing and leg exercises. These help prevent complications such as chest infections and blood clots in your legs and should be carried out every hour that you are awake and while on bed rest.
 Breathing Exercises: Take five long and slow deep breaths. Each breath should be deeper than the previous breath. Think about getting the air to the very bottom of your lungs.
Breathing Exercises: Take five long and slow deep breaths. Each breath should be deeper than the previous breath. Think about getting the air to the very bottom of your lungs.
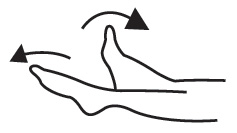
Circulation exercises: Firmly move your ankles up and down to stretch and contract your calf muscles.
Post-operative phase—days one to three
Mobility
The day following your surgery you will be assisted to mobilise by the nursing staff and/or your physiotherapist. By the second day after your surgery you should be able to mobilise independently, however your nurse can assist you to mobilise if you still need some support or supervision. It is important to move around in order to maintain good circulation and prevent complications. It is also advisable to plan quiet afternoons and rest. We suggest you limit your visitors.
Hygiene
The day following your surgery you will be assisted to shower by the nursing staff. By the second day after your surgery you should be able to shower independently. Please let your nurse know if you still need assistance.
Diet
You will progress from a fluid diet to a light/normal diet when advised by your doctor.
Treatments
You will need to continue wearing the anti embolic stockings for the duration of your stay in hospital and at home until the seventh day after your surgery.
The vaginal pack (if applicable) is usually removed the day following your surgery.
If you have a drain in your abdomen this will be removed the first or second day following your surgery.
Dressings
Your dressings will be removed when instructed by your surgeon. Once the dressings have been removed wash your wound with soapy water and pat dry.
Observations
Your vital signs, wound (if applicable) and vaginal discharge will be monitored regularly.
Medications
Your IV drip should be removed the day following your surgery. It will only remain in place longer if you are not tolerating an adequate oral intake or if medications are required intravenously.
Please tell your nurse if you have any pain or nausea, so these symptoms can be managed.
Your doctor may request that you continue on the anti-coagulant injections for five days after you go home; nursing staff will teach you how to administer this.
Elimination
Your urinary catheter will remain in place until the first or second day after your surgery. After the catheter has been removed nursing staff will request that you notify them each time you pass urine. The amount of urine passed will be measured and the nurse will then scan your bladder with an ultrasound device. This process is referred to as a "trial of void" and will identify if you are emptying your bladder properly. If your bladder is not emptying completely and you have had pelvic floor surgery or have had difficulty passing urine previously, you may need to be taught to self catheterise.
It is important to avoid straining when moving your bowels—you will be given regular medication to avoid constipation according to your surgeon's regime.
Consults
Your surgeon will visit daily to discuss your progress. If requested by your doctor a physiotherapist will visit you during your stay to provide advice and information on pelvic floor and any other exercises required to assist your recovery
Day of discharge—day two to four
- Discharge time is 10 am.
- A discharge summary form will be discussed and provided.
- Your own medications will be returned to you and any new ones supplied.
- Your X-rays will be returned to you. Please remember to ask for them.
- Your postoperative appointment will be discussed—this should be four to six weeks after your surgery.
What to expect after you go home
Pain management
You may require some mild pain relief for wound discomfort as ordered by your surgeon.
Wound management
Nursing staff will provide you with information re ongoing management of your wound (if applicable).
Activity
For the first two to three weeks after your surgery lift nothing greater than two kilograms. After this aim to increase your activity as you feel comfortable.
Refer to the information provided by your physiotherapist for further advice on suitable exercises.
Continue to wear the anti embolic stockings, especially overnight, for at least one to two weeks after your surgery.
Sexual intercourse should be avoided for four to six weeks or as advised by your doctor.
Nutrition
You should aim to drink between six to eight glasses of fluid per day—at least half of this should be water. This promotes good bladder and bowel function. Maintaining a healthy and nutritious diet will also aid your recovery.
Driving
You can usually resume driving about two weeks following surgery provided you are able to apply the brake heavily in an emergency and are able to comfortably steer and turn from side to side to check traffic. It is advisable to contact your car insurance company to find out when you are covered to drive again.
It is important to notify your surgeon if
- You notice any discharge from your wound or if it becomes red or inflamed
- you develop a fever (temperature above 38 degrees Celsius)
- you are bleeding vaginally heavier than a normal period
- you have pain that is not relieved by simple analgesia.
Contact
Mater Private Hospital Springfield
30 Health Care Drive, Springfield Central Q 4300
Telephone: 07 3098 3900
Website: www.mater.org.au
© 2015 Mater Misericordiae Ltd. ACN 096 708 922
Mater acknowledges consumer consultation in the development of this patient information.
Mater Doc Num: PI-CLN-460013
Last modified 25/9/2019.
Consumers were consulted in the development of this patient information.
Last consumer engagement date: 28/7/2015
For further translated health information, you can visit healthtranslations.vic.gov.au/ supported by the Victorian Department of Health and Human Services that offers a range of patient information in multiple languages.