Testing for Down syndrome and other chromosome abnormalities
Information for expectant parents
What are chromosome abnormalities?
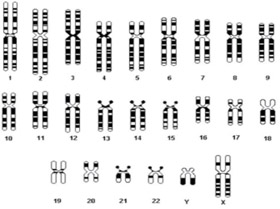
Chromosomes carry our individual genetic material (genes). Our bodies are made up of billions of cells, and in each cell there are 23 pairs of chromosomes. Extra or missing chromosomes may cause abnormalities that can affect a baby's development. The most common chromosome abnormality affecting newborns is Down syndrome which occurs in around 1 in 500 to 600 pregnancies.
Down syndrome (trisomy 21)
Down syndrome (also known as trisomy 21) is a genetic condition—it is not an illness or a disease. Down syndrome is caused by the occurrence of an extra chromosome; chromosome 21. This results in a range of physical features, health problems, developmental delay and some level of intellectual disability. In most cases there is no family history of Down syndrome as it usually occurs randomly. Other chromosome abnormalities such as Edward syndrome (trisomy 18) and Patau syndrome (trisomy 13) occur less often than Down syndrome but have more severe effects on the baby. Chromosome abnormalities cannot be reversed once they occur.
What tests are available?
- Screening test—looks for signs that a baby may be at an increased risk of having a chromosome abnormality, such as Down syndrome. A screening test cannot determine that a baby definitely has a certain abnormality. Screening tests do not carry any risk to the mother or baby.
- Diagnostic test—can confirm whether or not the baby is affected by certain chromosomal abnormalities. Diagnostic tests carry a small risk of pregnancy loss.
Screening tests
The First Trimester Combined Screen (FTCS)
The FTCS involves an ultrasound scan of the baby at 11 to 13 weeks gestation (nuchal translucency scan) and a blood test from the mother at 10 to 13 weeks gestation (Papp-A and BHcg). The test combines the mother's age (the age of the egg if using a donor egg), weight, ethnicity, smoking status, blood test results and ultrasound findings to indicate a level of risk for Down syndrome (trisomy 21), Edward syndrome (trisomy 18) and Patau syndrome (trisomy 13). Other markers such as the nasal bone may be included in the assessment.
The level of risk is described as a number e.g. 1 in 100 which is the same as a one per cent chance. A result is deemed high risk when it is more than 1 in 300 and low risk when less than 1 in 300.
Around five per cent of pregnant women (1 in 20) who have the FTCS will be given a 'high risk' result but the majority of them will not be carrying a baby with a chromosome abnormality. Within this 'high risk' group will be most cases of Down syndrome, Edward syndrome and Patau syndrome.
Around 95 per cent of pregnant women (19 in 20) who have the FTCS will be given a 'low risk' result. Within this 'low risk' group there will still be some cases of Down syndrome, Edward syndrome and Patau syndrome.

An ultrasound scan image showing the area at the back of the neck called the 'nuchal translucency'
The triple test or second trimester maternal serum screen
The triple test is a blood test performed in the second trimester of pregnancy at 15 to 20 weeks gestation. It measures the levels of certain hormones in the mother's blood to assess the risk of Down syndrome, Edward syndrome, Patau syndrome and also neural tube defects (e.g. spina bifida). Dating the pregnancy by ultrasound is recommended for the triple test.
Around five per cent of pregnant women (1 in 20) who have the triple test will be given a 'high risk' result but the majority of them will not be carrying a baby with a chromosome abnormality. Within this 'high risk' group will be most cases of Down syndrome.
Around 95 per cent of pregnant women (19 in 20) who have the triple test will be given a 'low risk' result. Within this 'low risk' group there will still be some cases of Down syndrome.
If the risk for a neural tube defect (spina bifida) is 'high', an ultrasound scan is recommended as the diagnostic test.
Non-invasive prenatal testing (NIPT)
NIPT involves taking a sample of blood from the pregnant woman. This can be done from 10 weeks of pregnancy onwards. The blood sample is evaluated for the baby’s DNA to determine a level of risk for Down syndrome (trisomy 21), Edward syndrome (trisomy 18) and Patau syndrome (trisomy 13).
It is important to understand that NIPT is a screening and not a diagnostic test. If the result comes back indicating a low risk for trisomies 21, 18 and 13, it is very unlikely (less than or equal to 0.1% chance) that your baby has one of these disorders. If the result comes back indicating a high risk of trisomy, invasive testing with amniocentesis or chorionic villus sampling may be offered. Furthermore, this test does not provide information about structural abnormalities. However, the benefit of the test is that it is non-invasive and not associated with an increased risk of pregnancy loss.
NIPT is offered to high-risk women including those aged 35 years and over, those with an abnormal ultrasound, a personal or family history of aneuploidy, and an abnormal CFTS or triple test. However, NIPT can also be performed for low-risk women.
This test can be performed for both singleton and twin pregnancies, although CFTS is the preferred test for twin pregnancies. For triplets and more, the nuchal translucency (NT) test and measurement of the nasal bone is the preferred option.
The turnaround time for NIPT results is up to 14 days. Up to five per cent (1 in 20) of NIPT tests may not return a result due to insufficient quantity of fetal DNA in the maternal blood sample.
Diagnostic tests
Chorionic Villus Sampling (CVS) and amniocentesis are both diagnostic tests that can confirm whether or not a baby has a chromosome abnormality. They involve sampling of the placenta (CVS) or amniotic fluid (amniocentesis) and carry a risk of pregnancy loss of between 0.5 and 1 per cent. For further information please see Mater's brochure: Chorionic Villus Sampling (CVS) and Amniocentesis.
Frequently asked questions
Should I have more than one screening test?
No. A screening test should only be performed once. The same screening test should not be repeated. A triple test is not required if a FTCS has already been performed.
Are there any benefits to testing?
Informing the parents about potential problems during the pregnancy is a normal part of providing good antenatal care. Babies with chromosome abnormalities may require monitoring before birth for specific abnormalities e.g. cardiac malformations. In some circumstances, birth may be required in a specialised centre. Knowledge of a chromosome abnormality affecting the unborn baby may also influence when and how the baby is born. Information about health problems affecting their unborn baby gives parents the opportunity to seek further information, counselling and support.
Are there any downsides to testing?
Parents should consider the risks and benefits of all antenatal tests before proceeding. Testing for health problems affecting the unborn baby may create an unwelcome level of anxiety for some parents and relief for others. Diagnostic testing carries a small risk of pregnancy loss that has to be weighed against the potential benefits of knowing early in pregnancy that a baby might have health problems. We encourage you to ask your health provider questions about the possible risks and benefits of any suggested treatment or tests, as well as the range of possible outcomes.
What about the 18 to 20 week scan?
It is recommended that all women have an ultrasound in pregnancy between 18+0 to 20+6 weeks to check for structural abnormalities, amniotic fluid volume and placental location. The 18 to 20 week scan is not recommended as a screening test for Down syndrome due to its poor performance.
What if testing indicates a problem?
Your health provider will discuss the results of the tests with you. They can also arrange referral for further counselling or additional testing if required.
Can all abnormalities be ruled out?
The majority of babies are healthy at birth. While some conditions such as Down syndrome can be tested for during pregnancy, not all abnormalities can be ruled out. If you have concerns about any specific conditions e.g. those that might be present in a family member, please discuss this with your health care provider.
How can I arrange to have testing?
The first thing to do is to discuss available testing options with your health care provider. FTCS is performed in most local radiology practices accredited to perform the nuchal translucency scan. The nuchal translucency scan usually incurs an out-of-pocket expense.
Mater Centre for Maternal Fetal Medicine (MFM)
As a tertiary referral centre MFM provides diagnostic testing by CVS or amniocentesis. Pre and post-procedure counselling is included as part of our service. Referrals for diagnostic testing by CVS or amniocentesis can be faxed to 07 3163 1890. A referral from a doctor is required to access services provided by the centre. Bulk-billing is available for public patients referred from Queensland Health Hospitals and those holding Health Care cards. An estimate of fees can be obtained by contacting our reception staff on 07 3163 1896.
Contact details
Mater Centre for Maternal Fetal Medicine
Level 7
Mater Mothers' Hospital
Raymond Terrace
South Brisbane Qld 4101
Phone: 07 3163 1896
Fax: 07 3163 1890
Website: www.matermothers.org.au
Further information and support
Genetic Health Queensland
Phone: 07 3636 1686
Website: http://www.health.qld.gov.au/ghq/default.asp
Down Syndrome Association of Qld
Phone: 07 3356 6655
Website: www.dsaq.org.au
Centre for Genetics Education
Website: www.genetics.edu.au
Fetal Medicine Foundation (UK)
Website: www.fetalmedicine.com
Mater acknowledges consumer consultation in the development of this patient information.
Mater Doc Num: PI-CLN-430139
Last modified 18/10/2017.
Consumers were consulted in the development of this patient information.
Last consumer engagement date: 22/8/2017
For further translated health information, you can visit healthtranslations.vic.gov.au/ supported by the Victorian Department of Health and Human Services that offers a range of patient information in multiple languages.