Women’s health—hysterectomy
Hysterectomy
We understand that having an operation can be a very stressful experience. This information aims to alleviate some of your concerns. It explains briefly what to expect before you come to hospital, the events that may occur during your stay and what to expect when you are discharged from hospital. However, this is a guide only, as each person may require differing treatments.
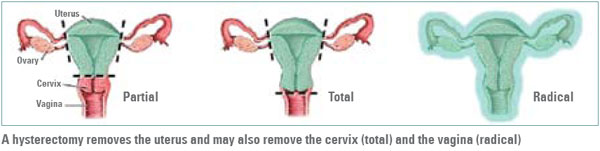
What is a hysterectomy?
A hysterectomy is an operation to remove the uterus and, usually, the cervix. The ovaries and tubes may or may not be removed during this procedure, depending on the reasons for the surgery being performed. If the ovaries are removed, you will commence menopause. A hysterectomy is a major surgical procedure with physical and psychological consequences.
Why is a hysterectomy performed?
Common reasons include painful or heavy periods, pelvic pain, fibroids or as a part
of therapy for cancer. You should have a clear understanding of your reason for this
surgery. If not, please ask your doctor.
What are the alternatives to this treatment?
A number of other conservative options may be appropriate for your particular
condition and will normally have been considered prior to your decision to undergo a
hysterectomy.
How is this done?
The procedure is normally performed under a general anaesthetic and takes approximately one hour. However, you can expect to be in theatre and recovery for up to three hours.
To commence your anaesthetic a drip is inserted into your arm. Once you are
asleep you will have a urinary catheter inserted. The importance of the catheter
is to reduce the size of your bladder, keeping it away from the operation site and
reducing the risk of complications. Once the catheter is inserted the operation
can commence.
There are three ways to remove the uterus:
- Vaginal hysterectomy—the removal of uterus and closing of the wound is performed through the vagina. There is no cut in the abdomen.
- Laparoscopic hysterectomy—about four small keyhole cuts are made in the abdomen to divide the attachments of uterus, ovaries and tubes in the pelvis. The uterus is usually then removed through the vagina.
- Abdominal hysterectomy—the uterus is removed through a cut in the lower abdomen. The cut is about 15–20 cm in length and runs across your abdomen, usually below the bikini line. Less commonly, it may be necessary to have a cut that runs from the belly button down to the pubic area.
What are the risks of undergoing this procedure?
Although the risks associated with hysterectomy are low, you should be aware
that every surgical procedure has some risk. This may also depend upon the
type of surgery you have.
Specific risks to be aware of in relation to vaginal hysterectomy, laparoscopic hysterectomy and abdominal hysterectomy include:
- Severe bleeding from large blood vessels around the uterus or top of vagina. This is not common. Emergency surgery may be required to repair the damaged blood vessels, or a blood transfusion may be required to replace blood loss. A vaginal pack may also be used to control the bleeding.
- Infection in the operation site, pelvis or urinary tract. Treatment may include antibiotics.
- Nearby organs such as the ureter (tube leading from kidney to bladder), bladder or bowel may be injured—expected to happen to approximately one in every 140 women. Further surgery will be needed to repair the injuries. For bladder injuries, a catheter may be put into the bladder to drain the urine away until the bladder is healed. For ureter injury, a plastic tube (stent) is placed in the ureter for some weeks.If the bowel is injured, part of the bowel may be removed with a possibility of a temporary or permanent colostomy (bag on the abdomen to collect faeces).
- The bowel may not work after the operation; this is usually temporary. Treatment may include a drip to give fluids into the vein and no food or fluids by mouth.
- Rarely, a connection (fistula) may develop between the bladder and the vagina. This causes uncontrollable leakage of urine into the vagina and requires further
corrective surgery.
- A change in the sensory nerves of the bladder and bowel. Constipation and
bladder problems may occur.
- Psychological changes may occur after surgery. Feelings of depression and
anxiety can be prolonged after surgery. Counselling may be of some benefit.
Specific risks to be aware of in relation to laparoscopic hysterectomy and abdominal hysterectomy wounds:
- Bleeding into the wound internally from surrounding blood vessels. A drain may be required to drain fluid from the wound and antibiotics may also be required.
- The layers of the wound may not heal well and the wound may open up. A hernia (weakness/hole in the deeper tissues) may form in the long term which may require repair by surgery. An infection may involve ongoing wound care with dressings and antibiotics.
- The scar can be thickened, red and may be painful. This can be disfiguring and may be permanent.
- Numbness under or around the wound is relatively common and, while it normally resolves, it may be permanent.
General risks during all operations:
- Small areas of the lungs may collapse, increasing the risk of chest infection. This may require antibiotics and physiotherapy.
- Clots in the legs with pain and swelling. Rarely, part of this clot may break off and go to the lungs which can be fatal.
- A heart attack because of strain on the heart or a stroke. Extremely rarely, death is a possibility in anyone undergoing an operation.
- Chronic abdominal pain related to internal scarring (adhesions).
Some women have an increased risk of complications:
- Women who are very overweight may have an increased wound infection, chest infection, heart and lung complications and blood clots.
- Smokers have an increased risk of wound and chest infections, heart and lung complications and blood clots.
Procedure planning day
When you had your appointments with your specialist, the case manager and the preadmission clinic, planning for your surgery began, including:
- an explanation of your surgery
- signing the consent form
- booking the date of your surgery
- estimation of the day you will be going home
- booking your post-operative six week follow-up appointment, or phone call
- the provision of information regarding your pre-operative physiotherapy
appointment
- discussion of your patient information booklet and its contents.
Below is a summary of your procedure plan and follow-up appointments:
Preoperative planning
- Date of surgery
- Date of admission (if different to surgery date)
- Expected length of hospital stay (laparoscopic or vaginal hysterectomy is two days . Abdominal hysterectomy is three days)
- Estimated date of discharge
- Surgeon
- Anaesthetist
- Case manager
- Pre-operative physiotherapy appointment
Postoperative consultations
- Specialist follow-up appointment (your specialist follow-up appointment is made in advance to guarantee you a booking time. As rescheduling is difficult we wish to suggest requests for rescheduling is limited to medical requests and unforeseen circumstances)
- Abdominal hysterectomy postoperative appointment
- Vaginal hysterectomy postoperative appointment
- Laparoscopic hysterectomy post-operative appointment
- Allied health follow-up appointments.
The assessments taken during your time with the case manager and the preadmission service provide important information on your health and social status allowing your particular needs to be identified and managed. Appropriate referrals will be made either prior to, or following, your surgery.
Things to do before you come to hospital
- It is important for you to have all the tests ordered at your outpatient clinic appointment completed prior to coming to hospital. Please bring X-rays, any ECG reports and all your blood test results with you to hospital, along with your medications. Your medications need to be in their labelled containers or Webster pack.
- If you are taking any blood thinning or arthritis medications please follow the instructions provided by your preadmission nurse or pharmacist, as sometimes it is important that these medications be stopped in preparation for your surgery. You should continue your regular medications, unless advised otherwise. If you are a smoker it is also important for you to stop smoking.
- It is important for you to be familiar with, and start practising, your breathing and leg exercises, which you will need to commence once you have woken up from your operation, and getting in and out of bed.
- You may be required to have a bowel preparation, which will empty your bowel prior to the surgery. If this is required, you should only have fluids (clear soups, jellies, cordials, juices or similar drinks) in the 24 hours prior to the surgery. The bowel preparation medication should be taken as prescribed.
- In some circumstances your surgery may need to be rescheduled or cancelled. If you are feeling unwell or have developed an illness we advise you to make an appointment with your GP who can then inform you if you are well enough to have surgery.
- If your surgery needs to be rescheduled or cancelled due to advice from a medical practitioner or unforseen personal circumstances please notify Bookings at Mater Health Services on telephone 07 3163 8244 as soon as possible and provide them with your name, the reason for the cancellation and if you require the surgery to be rescheduled.
- You should stop eating and drinking at the following times on the day of your surgery unless otherwise notified
- At midnight if your procedure is in the morning
- At 6 am if your procedure is in the afternoon.
- You will need to shower and dress into clean clothes prior to coming into hospital. While showering it is important to include cleaning your naval area well. No skin products such as deodorant, perfume, body lotion or powder are to be used following your shower. It is important that you do not shave your operation site as this increases the risk of wound infection.
- Please remove all body jewellery.
- As Mater is unable to accept liability for losses it is highly recommended that you leave your valuables at home for safety and security purposes. Please bring essential items only. While Mater does not take responsibility for your personal belongings our Security Office will hold any lost property that is handed in.
What to bring to hospital
- Toiletries
- Comfortable sleep-wear
- Underwear
- Sanitary pads
- All usual medications
- All X-rays
- Medicare card
- Your patient information booklet.
The day of your surgery
Before your surgery
- You will be admitted to hospital and prepared for surgery in the Day Procedure Unit, Level 5, Mater Adult Hospital, unless otherwise arranged.
- The assessment form completed at the preadmission service will be reviewed and your health team will plan for your individualised care while in hospital, discuss any concern you may have and support you may require after discharge. If any changes to your circumstances have occurred since the preadmission interview, please notify your nurse. Your nurse will also check that your consent form has been signed, or organise for it to be signed, before your operation.
- It is an infection control requirement at Mater that you will be required to have swabs taken if you have transferred from, or worked at, another health care facility or you have had previous resistant infections. This is usually identified, and attended to, at the preadmission clinic. Your admission nurse will check if these three swabs have been taken and will complete the test if there are further swabs required.
- The medications you brought to hospital will be collected. Please remember to ask for these to be returned to you when you leave the hospital. Please inform the nurse admitting you if you have been taking any blood thinning, arthritis medication or aspirin prior to your admission, as these may have needed to be stopped before your operation day. It is usual for you to continue taking your other prescribed medications.
- You may walk as much as you like up until two hours prior to your surgery. Please notify staff if you leave the ward.
- You will have an identification armband applied. This will stay on for the duration of your stay for identification and safety reasons. If you have any known allergies, you will have an allergy armband applied.
- Your nurse will take a set of baseline observations, weigh you and may ask you to provide a urine sample for routine testing.
- It may be necessary to clip any hair in the surgical area.
- You will be asked to dress into theatre clothing.
- You will be measured for special stockings and will need to have these put on prior to going to theatre. Also a compression device will be applied to your legs approximately two hours prior to your operation. These assist with blood flow through your legs and decrease the risk of blood clot formation while you have decreased mobility.
- You may be prescribed a pre-anaesthetic medication before you go to surgery.
- Before you leave for theatre a pre-operative checklist will be completed with you by your nurse. This checklist will be repeated in the operating reception area. Apart from your wedding band, which will be covered with tape, no jewellery or metal is to be worn to theatre.
- It is important to continue practising your breathing and leg exercises which you will need to commence once you have woken up from your operation.
After your surgery
- When you wake from the anaesthetic, you will be ready to be transferred, in your bed, from recovery to your hospital room.
- It is important for you to start your breathing and leg (circulation) exercises. These exercises help prevent complications such as chest infections and blood clots in your legs:
Breathing exercises
Every hour you are awake and while resting in bed take five long and slow deep breaths. Each breath should be deeper than the previous breath. Think about getting the air to the very bottom of your lungs.
Taking a deep breath may trigger a cough. Support your wound with your hands and forearms; perhaps use a pillow over your tummy to protect as you cough. Bent knees help to reduce further strain on your wound.
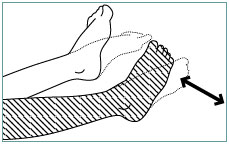 Leg exercises
Leg exercises
These exercises improve the blood circulation and may help prevent blood clots from forming in the legs. Start doing this exercise in bed and then once you start sitting out of bed.
- Move your feet up and down briskly from your ankles.
- While your leg is straight, push your knee gently into the bed and pull your toes towards your head. Hold this stretch for a few seconds and then relax. Repeat five times with each leg if comfortable.
- Squeeze your buttocks tightly and then relax. Repeat a few times.
- Having an anaesthetic can make you feel sick and may cause vomiting. You will have a drip in your arm which is necessary to maintain fluid intake and provide pain relief. This will remain in until you are tolerating food and fluids and your pain control is changed to oral medication.
- Your nurse will take frequent observations of your vital signs e.g. temperature, pulse, blood pressure, wound dressing and drain for several hours after the surgery. As you recover, these observations become less frequent although remain regular until you leave hospital. Vaginal bleeding will also be monitored.
- You will receive oxygen while you are waking from the anaesthetic and while you receive your pain medication through your drip.
- Immediately following your surgery, you will be resting in bed. Your nurse will assist you to freshen-up following your surgery and when you feel well enough you will be assisted the first time you get out of bed.
- You may have small amounts of water or ice to suck, then progress from fluids to a normal diet as tolerated.
- If you have pain or nausea, please tell your nurse. Effective pain management is important. Remember when you have pain, you are less likely to breathe deeply and more likely to withhold coughing and movement.
- You will have a urinary catheter in place. The catheter will normally be removed the day following your surgery.
- Wound care:
- Abdominal hysterectomy—a dressing will cover your wound which is closed with either stitches or staples. You may also have a drain inserted close to your wound which will remove excess blood and fluid from the surgical area.
- Vaginal hysterectomy—you may have a vaginal pack in place. This acts as a large tampon. It can cause discomfort and is usually removed after 24 hours. It is not painful when it is removed.
- Laparoscopic hysterectomy—Small dressings will cover your key-hole incision sites which will be closed with either glue or sutures.
- You may also have a drain inserted close to your wound. The purpose of the drain is to remove blood and fluid from your wound.
Vaginal/laparoscopic hysterectomy—day one post-operatively
Abdominal hysterectomy—days one to two postoperatively
You should expect that:
- your pulse, blood pressure and temperature will be within the normal range
- pain relief will maintain your comfort
- you may have a blood test to check your haemoglobin (iron) level
- your IV treatment will be discontinued if you are tolerating your diet and fluids and your blood tests are normal
- you will have progressed to and be tolerating, a normal diet
- you will have your catheter removed and your urine output will be monitored closely
- you will be encouraged to slowly increase mobilisation, getting in and out of bed through side-lying (see below).
Wound care
- Abdominal hysterectomy—your dressing will remain intact as this reduces the risk of infection. Your drains will be removed upon your doctor’s instruction. Your vaginal loss will be scant.
- Vaginal hysterectomy—your vaginal pack will be removed and your blood loss will be similar to a light period.
- Laparoscopic hysterectomy—your vaginal loss will be scant.
Observations
Nurses will continue to take your observations regularly (temperature, pulse, blood pressure) and monitor your wound, dressing, drain and vaginal bleeding.
Medications
You will be given your regular medications today, plus any required for pain relief. Please let the nursing staff know when you have pain.
Treatment
You will have the compression stockings on your legs removed once you are getting out of bed. You will continue to wear the special stockings if ordered. Some women will receive an injection of heparin to reduce the risk of developing blood clots in the legs.
Mobility
Following instructions provided by your surgical team, your movement in and out of bed and around the ward will increase slowly each day. It is important to follow your physiotherapist’s instructions when moving in and out of bed.
Getting in and out of bed through side-lying
- Gently brace as demonstrated by the physiotherapist preoperatively. Bracing involves gentle activation of pelvic floor muscles and deep tummy muscles.
- Make sure the bed is flat. Draw in the pelvic floor as you bend both knees up, one at a time.
- Roll over to your side without twisting too much and keep your knees bent.
- With your top arm well in front of you, push your upper body forward and up, as you allow your legs to go down at the same time.
- Remember to keep breathing, keep your knees bent, and come forward and up to sitting in one smooth action.
- Always try to stand tall, with your shoulders relaxed as you walk.

If you have any symptoms of pelvic floor weakness or are unsure how to activate these muscles, phone the Physiotherapy Department on telephone 07 3163 8787.
Nutrition
Once you are tolerating 500 ml or more of fluid you will be able to commence eating your normal diet.
Hygiene
- Showering/bathing
- Abdominal hysterectomy—you may be well enough to be assisted with having a shower on the first day following your surgery. Alternatively you will be given a sponge in bed. On the second day following your surgery you will be encouraged to shower independently.
- Vaginal/laparoscopic hysterectomy—you will be assisted as needed with having a shower.
- For your toileting needs you will be given assistance as needed and encouraged to increase your independence.
- Your urine will be measured following the removal of your catheter to ensure your bladder is functioning adequately.
Education and emotional support
- Your nurse will discuss this information with you and ensure you understand your care. Please take the opportunity to discuss any concerns you have with your nurse.
- If you have any questions about your treatment please ask your doctor or nurse. Our pastoral care team offers a caring support network to all patients. The dedicated members of this team will visit you during your stay and are available, at your request, to discuss any anxieties or problems that you may have.
Discharge planning
Planning for your discharge begins with your admission. If your recovery has been without complications your discharge day will be the second or third day following surgery depending on your type of hysterectomy. Your doctor will confirm this with you.
Day of discharge
You should expect that:
- your temperature will be within normal limits
- your vaginal loss will be minimal
- your wounds will be healing and there will be no signs of infection, inflammation or unexpected bleeding
- you will be comfortable and your pain will be managed with oral medication
- you will understand all education provided and your plan of care after leaving hospital
- you are able to walk independently to an appropriate level for home activity
- you are able to tolerate fluids and diet.
Activities of daily living
- It is expected you will be mobilising independently to an appropriate level for home activity. At home mobilise around the house and yard initially, then go for short walks. Aim to gradually increase your activity every day. By four weeks you should be fully mobile.
- Your bowel and bladder functions should continue to return to normal.
- Have a shower and avoid a bath.
- You may have foods and fluids as desired. A diet promoting tissue healing, including protein, iron and vitamin C is recommended. A high fibre diet along with two to three litres of fluid each day will encourage bowel regularity.
Medications
- You will continue to take your regular medications. If there are specific discharge medications required they will be given to you along with relevant advice.
- For pain control you may use paracetamol (Panadol) and other medication as ordered by your doctor. Please ensure you follow your doctor's instructions when using any pain medication.
Treatments
- You will need to continue to wear your stockings, especially overnight, for one to two weeks.
- Wound care: abdominal/laparoscopic hysterectomy—if your dressings are removed you may leave your wound exposed. If your dressings are left intact, instructions will be given to you about when, and how, to remove your dressings. As part of your discharge plan you will be advised to make an appointment with your GP to have a wound check two weeks after your surgery.
Education and discharge plan
- Opportunity will be provided for you to discuss any concerns and emotional needs.
- Your nurse will confirm you understand all your education, discharge advice and discharge plan.
Recovering at home
What to expect
- You may have a blood stained vaginal discharge which is similar to a light period. This will gradually reduce to nil over the fortnight as your internal wound heals.
- You may need to take some simple analgesia for pain/discomfort, especially on waking and settling at night.
- You may feel fatigued.
- It is normal to experience some depression after this procedure.
- You may require up to four to six weeks off work. You should have returned to normal activity by two to three months, depending on the type of surgery, although full recovery may take longer.
- After the operation you will no longer be able to have children. Even if you have not yet gone through menopause, you will no longer have periods.
- For the majority of women hysterectomy surgery does not have a negative effect on sexual function.
What to avoid
- For the first two to three weeks lift nothing greater than two kilograms. Increase gently as tolerated over six weeks.
- It will take about three weeks before you should drive a car. Only when you know you can act confidently with emergency breaking should you attempt driving the car.
- Avoid sexual intercourse for six weeks to allow healing to take place.
- Avoid inserting anything into the vagina for six weeks to allow time for healing to take place (e.g. use sanitary pads and not tampons).
 The lean forward position has been shown to assist in opening the bowels with more ease and helps to prevent straining (see diagram).
The lean forward position has been shown to assist in opening the bowels with more ease and helps to prevent straining (see diagram).
- Lean forward from the hips.
- Lean through your forearms.
- Come up on the balls of your feet if comfortable.
- Allow your abdomen to relax forward.
- Do not hold your breath or strain.
- A small footstool may enhance the position.
It is important to avoid constipation and straining immediately after your surgery as this will assist healing and improve your comfort. Maintaining your bowel motion consistency (soft and easy to pass) long term will lessen the chance of prolapse and incontinence in the future.
Contact
- All general hospital enquiries please contact: 07 3163 8664.
- For all queries related to your up-coming surgery please contact the Women’s Health Unit Case Manager Monday to Friday between 8 am and 4 pm on telephone 07 3163 3000
- For post-operative complications as listed below please contact
- Mater Adult Hospital Emergency Department on telephone 07 3163 8111
- your GP.
Complications
- Your wound becomes red or inflamed, painful.
- You have heavy vaginal bleeding—heavier than a normal period.
- You have offensive vaginal discharge.
- You develop a fever i.e. temperature about 38° C, or you are feeling unwell.
- You have pain that is not relieved by simple analgesia.
- Nausea and vomiting that is difficult to manage.
- You are having difficulty passing urine or opening your bowels.
Reference
2008 Inpatient and Surgical Care/Ambulatory surgery/Home Care 12th edn Milliman Care Guidelines.
© 2014 Mater Misericordiae Ltd. ACN 096 708 922.
Mater acknowledges consumer consultation in the development of this patient information.
Mater Doc Num: PI-CLN-460013
Last modified 25/9/2019.
Consumers were consulted in the development of this patient information.
Last consumer engagement date: 20/1/2014
For further translated health information, you can visit healthtranslations.vic.gov.au/ supported by the Victorian Department of Health and Human Services that offers a range of patient information in multiple languages.