Abdominoperineal resection/total colectomy with proctectomy
Welcome
At Mater, we understand that having an operation can be a very stressful experience. This booklet aims to alleviate some of your concerns, in keeping with our Mission to offer compassionate, quality care that promotes dignity while responding to patients' needs. It explains the general day to day events that may occur during your visit and the things to expect following your discharge.
Each person may require different treatments. This booklet is intended as a guide only.
If you have any questions about your treatment please ask your doctor or nurse. Our pastoral care team offers a caring support network to all patients. The dedicated members of this team will visit you during your stay and are available to discuss any anxieties or problems at your request.
Abdominoperineal resection/total colectomy with proctectomy
Both these surgeries are performed to remove bowel disease affecting different parts of the large bowel. The choice of surgery is dependent on where the growth or disease extends to.
The abdomino-perineal resection involves removing a section of large bowel (the sigmoid colon) along with the rectum and the anus (the back passage).
The total colectomy with proctectomy involves removing the entire large bowel along with the rectum and anus (the back passage). When the back passage is removed, the area is then stitched up and permanently closed. A new permanent opening for the bowel is called a stoma and is made in the wall of the abdomen (tummy). Bo dy waste then collects in a disposable adhesive bag which covers the new stoma.
If you are undergoing the abdomino-perineal resection, the stoma is called a 'colostomy' because it is formed in the remaining section of the large bowel (colon). If you are undergoing a total colectomy with proctectomy, the stoma is called an 'Ileostomy' because it is formed in the small bowel (ileum), as the large bowel has been completely removed.
Expected length of hospital stay
Abdominoperineal resection/total colectomy with proctectomy has a hospital length of stay of approximately seven days.
Benefits of having the surgery
Removing the diseased bowel is the first treatment for a tumour or inflammation of the bowel aiming to provide you with the best chance of a cure or significant improvement in your bowel problems. It is important to know that your recovery does depend on how far the disease has spread at the time of your surgery.
What risks are involved with this surgery?
Bowel surgery is classified as a major surgery and can carry a risk to your life. Your surgeon would have discussed this risk with you.
Most people will not experience any serious complication from their surgery, however, risks do increase with age and for those who already have heart, chest, and other medical conditions such as diabetes or if you are overweight or smoke.
After any major operation there is a risk of:
- chest infection: this risk can be minimised by practising deep breathing exercises and following the instructions of your nurse or physiotherapist. If you smoke, we strongly advise you to stop
- wound infection: this risk is increased with bowel surgery. One reason for cleansing of the bowel prior to surgery is to reduce the risk of any bowel leakage into your abdomen which could then lead to wound breakdown and infection. Antibiotics are usually given through a drip at the time of surgery to help reduce this risk
- thrombosis (blood clot in the leg): major surgery carries a risk of blood clotting in the leg. To prevent this from occurring you will be given an injection once or twice a day of a blood thinning agent. This will continue until you go home. Moving around as much as you are able and regularly exercising your legs will also help reduce this risk. You will also be fitted with support stockings as a preventative measure to blood clot formation. Once again, if you smoke, we strongly advise you to stop
- pulmonary embolism (blood clot in the lungs): it is very rare that a blood clot will dislodge in the legs and travel to the lungs
- bleeding: a blood transfusion may be needed. Very rarely would further surgery be required
Risks specific to this operation
Ileus (paralysis of the bowel and small bowel obstruction)
Sometimes the bowel is slow to start working after surgery (ileus) or can be obstructed. If this happens the bowel may need to be rested and a drip is used to replace fluids (instead of you drinking). In addition you may need a nasogastric tube (tube in your nose which is passed into your stomach) which will prevent vomiting. These remain in place until the bowel starts functioning again.
Possible stoma problems
- Loss of blood supply—the blood supply to the stoma may fail and cause damage to the bowel. This may require further surgery.
- Stoma prolapse—stomal prolapse occurs when some of the bowel sticks out too far past the skin. For minor prolapses no treatment is needed. For more serious cases, further surgery may be required.
- Parastomal hernia—this is when the bowel pushes through a weak point in the muscle wall, bulging the skin near the stoma and causing pain. Minor hernias may not need any treatment but large hernias may require surgery.
- Irritation of the skin—local skin irritation around the stoma, including reddening of the skin and a rash, may occur for a variety of reasons. Your stomal therapy nurse will assist you with these problems.
Sexual problems
Following surgery, some men may be unable to obtain or sustain an erection. It may also mean that they cannot ejaculate. Women may experience pain during and after intercourse. Time may improve this condition for both men and women. Counselling may also be beneficial. For women, use of water-soluble lubricants during intercourse may help.
Damage to the ureter during surgery
This rarely this occurs and may mean further surgery is required.
After your operation
- You will stay in the recovery room within the theatre suite after the operation. When you have woken from the anaesthetic and are stable you will be transferred on your bed to your room.
- You will have a dressing over your wound. You may also have some drains; these remove excess fluid from the site of your operation and are usually removed two day or three after your operation.
- Your nurse will frequently monitor your vital signs (e.g. temperature, pulse and respirations, blood pressure etc.) drains, dressing and stoma for several hours after the surgery. As you become fully recovered, these observations become less frequent but remain regular until you leave hospital.
- Immediately following your surgery, you will be resting in bed. It is important to regularly do your breathing, coughing and leg exercises.
The following exercises help prevent complications suchas chest infections and blood clots in your legs. You should do these every hour that you are awake while resting in bed.
Breathing exercises: take five long and slow deep breaths. Each breath should be deeper than the previous breath. Think about getting the air to the very bottom of your lungs.
Circulation exercises: firmly move your ankles up and down to stretch and contract your calf muscles.
- Following your surgery it is also important to move as much as possible turning yourself from side to side, with the help of your nurse, if required. This will help circulation to all body parts and stop sore, red areas developing, especially on your bottom or heels.
- Your nurse will assist you to have a wash sometime after you return to the ward and assist you with hygiene cares.
- Immediately following your surgery it is recommended that you do not take anything orally for up to four hours. After four hours you will be provided with fluids and supplement drinks to assist in your recovery.
- You may continue some of your usual medications as ordered by your doctor. You may also be given an injection once or twice a day of blood thinning medication. This helps to prevent blood clots.
- Pain relief: you will have either a Patient Controlled Analgesia (PCA) or an epidural
- a PCA allows you to manage your own pain. PCA involves specialised equipment which is connected to a drip (IV). You will have a button to push which allows a small amount of pain relieving medication to be delivered directly into your vein via the drip. The equipment has a specialised safety program to reduce the risk of you receiving too much medication. You will remain on PCA until you are able to eat and drink. Your pain will then be managed with tablets. There is no risk of becoming addicted to strong pain relieving medication when it's used appropriately.
- an epidural delivers pain-relieving medication into the space in your spine where the nerves carry pain signals from your operation site to your spinal cord and brain. The epidural usually remains in for two to three days depending on your type of surgery. Some patients will experience little or no pain with an epidural and may feel numb around the operation site. This is quite normal as this is its intended effect and means that the epidural is working, however if pain is moderate or severe you must notify the nurses straight away. You must also notify the nurses if you have any feeling of numbness or tingling around your mouth or upper limbs.
- if you have a PCA or epidural, you will more than likely be prescribed paracetamol (Panadol®) four times a day. Paracetamol works well when used on a regular basis and helps to reduce the amount of stronger pain-relieving medication you require which therefore reduces their side effects.
- You will be given oxygen via nasal prongs or a mask while you have the epidural or PCA in place. It is important to always keep this on when sleeping.
- While we try to relieve your pain as much as possible, some times it is not possible to take your pain away completely. However, your pain must be controlled well enough for you to move, do your physiotherapy exercises and to sleep. If your pain relief is not adequately controlled for this please tell your nurse. Also tell your nurse if you have an itch, you feel nauseated or feel like vomiting. These may be side effects of the pain relieving medication and are usually easily managed.
- To maintain your fluid intake you will be receiving fluids via a drip (IV). This will be removed when you are tolerating adequate amounts of oral fluids.
- You will have a catheter (IDC) in your bladder to drain your urine; your nurse will monitor this every hour.
- You may have a tube in your nose called a naso-gastric tube. This drains away the gastric fluid from your stomach and rests your bowel. Your nurse will be caring for this regularly.
- The stockings and compression sleeves will remain on.
Continued post-operative care
Consults
- You will be visited by the medical team throughout your hospital stay and they will identify the day you will be discharged
- The Acute Pain Service will also be visiting you assessing your pain management on a daily basis.
- Your physiotherapist will visit you daily, increasing your mobility to allow for your safe discharge home.
- Your stomal therapist will also visit with you regularly gradually increasing your independence with managing your stoma.
- Your dietitian will visit you to ensure you are managing a nourishing diet and provide stoma nutrition education.
Emotional support and education
- If you or your family have any concerns or questions throughout your hospital stay, do not hesitate to talk with your nurse who can assist you or refer you to the pastoral care service.
- As you progress each day your doctor, nurse, physiotherapist and/or stomal therapist will provide you with instructions regarding treatment, mobility, stomal care and your ongoing care beyond discharge.
Tests and procedures
- Further tests and procedure will be ordered by your doctor as needed.
Observations
- Your nurse will continue taking your vital signs, stomal assessment along with wound and drain observations. As you recover these will become less frequent but remain regular until you leave hospital.
Medications
- Pain control—your PCA/epidural medication will remain in place through to day three or four. Oxygen therapy will continue while you have your pain control infusion. On ceasing the pain control infusion your pain will be managed on oral medication. It is very important to take this medication as ordered as controlling your pain will assist you in your mobility. It is important to inform your nurse if you are in pain or if your pain increases. Many patients after this type of surgery experience "wind" pain. This is quite natural and is associated with your bowel getting back to normal. Wind pain is best treated by using natural remedies such as peppermint water or peppermint tea so tell your nurse if this becomes a problem.
- IV therapy—your IV therapy will continue through to day three or four. Antibiotics are given through this fluid and your IV therapy will be removed upon medical orders once you are able to drink enough fluids to keep hydrated.
- Nausea control—medication will be made available to you if you are feeling sick or are vomiting. It is important to notify the nurses the minute you become nauseated because it is much easier to control if treated early. If the nurse gives you medication for nauseousness let them know if its not been relieved as there are alternative options for treatment.
Diet
- Unless ordered otherwise, your diet will commence as a fluid diet with three supplements on the day of surgery. If you are tolerating fluids by day one following surgery you will be offered a light diet with ongoing supplement drinks between meals. This diet will continue through to when you go home.
Treatments
- NG tube—you may have a naso-gastric tube in place which will be removed day one or two after your surgery depending your bowel recovery.
- Drains—your drains will remain in place for approximately two to three days following your surgery. The removal of your drains will be dependent on the amount of drainage. They are regularly monitored and will be removed upon medical orders.
- Wound—the doctor and nurses will assist with the care of the wound/s and changing of the dressing/s. If there is fluid leaking from around your dressing, please inform the nurses. You will be provided with instructions for ongoing wound care prior to discharge.
- TEDs/SCDs—TED stockings are to remain in place throughout your entire hospital stay. Nursing staff will conduct regular checks of your skin to ensure circulation is adequate. Stockings will be removed for showering and pressure care, then reapplied. As you become more mobile the SCDs will cease to be applied.
- Urinary catheter—your catheter will remain in place for approximately three to four days following your surgery. It is important for your nurse to measure your urine output regularly. On return from theatre your urine output will be measured 1/24. As your condition stabilises your urine output measure will be changed to 4/24 and then 8/24 before it is removed approximately day three or day four.
- Stomal care—initially your stomal therapist and nurse will be attending to your stoma care. From day two, stomal education will commence to progress you slowly to independence prior to you going home.
Hygiene
- Your nurse will assess your condition which will determine whether you will have a shower or a sponge the first day following your surgery. Showering with assistance will continue and you will be encouraged to shower independently by day five.
Mobility
- While on bed rest remember to keep up your deep breathing and circulation exercises. It is also important to support your wound when you cough.
- From day one your physiotherapist will be encouraging you to mobilise. Gradual increase in mobilisation will be encouraged until you have reached independence by about day four to five. Sitting out of bed will also be encouraged but only for a maximum period of 30 minutes. It is important for you to use a recliner chair and sit in the reclined position with no pressure on your perineal wound. By the time you are ready to go home you will be independent with your daily activities.
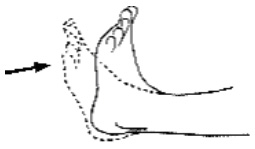
Getting in and out of bed through side lying
- Gently brace as demonstrated by the physiotherapist. Bracing involves gentle activation of pelvic floor muscles and deep tummy muscles.
- Make sure the bed is flat: draw in the pelvic floor as you bend both knees up one at a time.
- Roll over to your side without twisting too much and keep your knees bent.
- With your top arm well in front of you, push your upper body forward and up, as you allow your legs to go down at the same time.
- Remember to keep breathing, keep your knees bent, and come forward and up to sitting in one smooth action.
- Always try to stand tall, with your shoulders relaxed as you walk.

Discharge advice following bowel resection
What to expect
- some pain/discomfort at your wound site/abdomen for which you can take simple pain relief e.g. paracetamol—however do not take any more than eight tablets within a 24 hour period. Pain will subside as healing takes place
- some redness around wound and staples
- you may notice you may have a poor appetite for some time
- postoperative lethargy for a month or more
- some diarrhoea for a period of time after your surgery.
What to do
- maintain a nutritious diet as advised by your health care team
- maintain adequate fluid intake (avoid carbonated fluids)
- maintain your mobility at home and continue the breathing and circulation exercises and support your wound when you cough
- resume your normal sexual activity when you like.
What to avoid
- excessive activity/over exertion and heavy lifting
- pain relieving medication with codeine e.g. Panadeine ®, as they cause constipation
- constipation—eat a nutritious diet and drink plenty of water.
Please contact: Mater Hospital Brisbane Day Procedure Unit on 07 3163 8324, Mater Hospital Brisbane Emergency Department on 07 3163 8111 or your GP if any of the following occur after discharge:
- increase in swelling, redness or discharge from the wound
- a fever
- a marked increase in pain that is not relieved with simple analgesia, e.g. Panadol ® (do not take any more than eight tablets within a 24 hour period)
- nausea and vomiting which does not settle
- diarrhoea continues and becomes a problem to your lifestyle
- your stoma stops working
- you are experiencing abdominal distension
- there is a large amounts of bloody leakage from your wound
- blood is in your stool.

Acknowledgments
Staff of Mater Hospital Brisbane, Raymond Terrace, South Brisbane, Qld 4101
Copyright © 2010 Misericordiae Health Services Brisbane Limited ACN 096 708 922
Mater acknowledges consumer consultation in the development of this patient information.
Mater Doc Num: PI-CLN-420000
Last modified 28/5/2019.
Consumers were consulted in the development of this patient information.
Last consumer engagement date: 11/4/2015
For further translated health information, you can visit healthtranslations.vic.gov.au/ supported by the Victorian Department of Health and Human Services that offers a range of patient information in multiple languages.